BUDD CHIARI SYNDROME
Patient Education Material
liver
liver the largest solid organ in the human body. It lies within the tummy on the right side of the ribs, just below the lungs. The liver has two lobes and further divided into 8 segments.
The liver and bile duct system
Unlike other organs in the human body, the liver’s blood supply double by two vessels that supply blood, oxygen, and nutrients. The portal vein brings blood from the digestive system and accounts for 70-80% of the liver’s blood supply. The hepatic artery carries 20-30% of blood to the liver. Liver tumors get to take blood supply from branches of the hepatic artery. The liver your body’s metabolic factory and helps to control more than 500 chemical reactions, including:
- Storing carbohydrates.
- Breaking down proteins.
- Converting ammonia to urea a substance found in urine.
- Using fats to provide energy.
- Producing cholesterol which needed for the production of bile (which in turn helps to digest fats in the food) and hormones.
- Storing minerals and vitamins.
- Processing blood (breaking down old red blood cells and producing clotting factors).
Budd-Chiari syndrome:
Budd-Chiari syndrome (BCS) a disorder affecting the liver and blood vessels. where blood flowing into the liver difficulty in being able to flow out. leading to serious complications. Budd-Chiari Syndrome takes its name from George Budd. the English doctor who described the first cases in 1845, and Hans Chiari. the Austrian pathologist who credited with providing the first description of how it affects the body in 1899.
Blood flows into the liver from two blood vessels – the portal vein and the hepatic artery. After blood passed through the liver, it flows out through the hepatic veins and into the inferior vena cava. a large blood vessel that carries blood back to the heart. In Budd-Chiari syndrome, this flow partially blocked.
More about Budd-Chiari syndrome:
The immediate result a build-up (congestion) of blood in the liver. As there more flowing in than flowing out. The liver becomes swollen, tender to the touch, and a source of discomfort. The congestion causes fluid to leak from the liver into the abdominal cavity. The resulting build-up of fluid in the abdominal area called ascites. one of the commonest symptoms of Budd-Chiari syndrome. It may visible as a bulge in your tummy area and can uncomfortable and make it hard to breathe and eat normally.
If the blockage extensive and also affects the inferior vena cava. There may other places that become swollen. This particularly likely in the ankles and legs and called peripheral edema.
Causes of Budd-Chiari syndrome:
Blood contains a large number of elements. which maintain the delicate balance between being able to stop bleeding from a wound on the one hand and clotting too quickly or unnecessarily on the other. The obstruction in the veins in Budd-Chiari syndrome usually due to an imbalance in this system. where the blood clots too readily. Clots in blood vessels called thromboses and the condition where they’re a problem with blood clots called thrombotic disease. In 80% of patients with Budd-Chiari syndrome a condition that makes them more prone to thrombosis.
Blood (haematological) disorders:
Blood disorders the most common causes of Budd-Chiari syndrome. The most common one a group of conditions known together as myeloproliferative neoplasms (MPN). which affect around half of all patients with Budd-Chiari syndrome. MPN consists of three disorders called
- Polycythaemia vera,
- Essential thrombocythaemia
These patients often have acquired gene mutations in their blood cells which can now easily diagnosed with a blood test. The most common mutation known as the JAK2 mutation.
Paroxysmal nocturnal haemoglobinuria.
A number of non-haematological conditions or factors also linked with Budd-Chiari syndrome, including:
- Tumours, most commonly liver cancer or hepatocellular carcinoma (HCC).
- Chronic inflammatory diseases, such as Behçet disease, Sjögren syndrome or inflammatory bowel disease (IBD).
- Pregnancy
- High dose oestrogen from using oral contraception.
- Abscess, cyst or tumour can place direct pressure on your veins and increase the likelihood of a clot developing. This means that many existing disorders can complicate by Budd- Chiari syndrome.
- Web-like structures, called ‘membranous webs’, found in the major hepatic veins or inferior vena cava, far more commonly in South-east Asia.
More about causes of Budd Chiari syndrome:
Also frequently results in yellowing of the skin and eyes, known as jaundice. This due to the congestion and swelling of the liver.
Another effect less visible but also serious. This is called portal hypertension, where the blood pressure in the portal vein increased, because of the blockage in the blood coming out of the liver. As happens elsewhere in the body, blocked veins cause collateral vessels to enlarge (dilate) to provide an escape route for the obstructed blood. In portal hypertension, blood may return to the heart by using extra (dilated) veins lining your oesophagus (gullet) and stomach where they are known as varices. These veins have fragile walls, which cannot easily handle the increased blood flow and may burst. This leads to internal bleeding and referred to as ‘bleeding oesophageal varices’ which a medical emergency. A rare side effect of severe portal hypertension the development of confusion or even coma in severe Budd-Chiari syndrome. This is known as hepatic encephalopathy. See our leaflet on Hepatic Encephalopathy for more information.
There a range of treatment options available for Budd-Chiari syndrome, and essential that it diagnosed early before it causes liver damage or even liver failure. Early treatment can prevent liver failure, which may require an emergency liver transplant.
However, the disorder very rare. It affects between 1 and 4 people in 1 million in Western Europe. Budd-Chiari syndrome occurs in people from all ethnic backgrounds and affects young females more frequently.
Acute presentation:
Budd-Chiari syndrome can appear or ‘present’ as an acute condition which develops rapidly with the following symptoms:
- Abdominal pain in the upper right-hand side of your abdomen.
- Ascites (water in the belly).
- An enlarged liver due to the build-up of blood (hepatomegaly).
- swelling of legs and ankles
- Cramp in legs and feet
- Itching
Chronic Presentation:
More commonly, Budd-Chiari syndrome can develop in a chronic form. where people likely to have longstanding ascites and an enlarged liver (hepatomegaly).
Fulminant form:
Very rarely, there a fulminant form. This a type of disease with a sudden and severe onset. In fulminant Budd-Chiari syndrome, ascites, hepatomegaly, and kidney failure can occur with rapid liver failure.
Blood tests:
Including LFT’s, CBC, Clotting profile, and also a blood test to identify the underlying blood disorder
Ultrasound directs sound waves through your skin via a probe device as it passed over your liver area. In Budd-Chiari syndrome it used to obtain information about blood flow in your arteries and veins and this often gives enough information for the condition to diagnose.
A CT or MRI scan
A CT or MRI scan may also use. This can obtain pictures from different angles around your body using computer processing and can also show cross-sections of your tissue and organs. This scan can show an enlargement of the liver and changes in the density of liver tissue due to abnormal blood flow. A liver biopsy may necessary if other tests have helped doctors to identify the reason for liver problems.
Treatment
The aim of treatment for Budd-Chiari syndrome to keep your liver function stable by maintaining the flow of blood out of the liver. It very important that all patients with Budd-Chiari syndrome are treated in specialized hospitals with the required expertise, by a multidisciplinary team. This team of doctors includes liver specialists, blood disorder specialists (hematologists), and radiologists. They will look to:
- re-channel the blocked veins if possible.
- prevent recurrence or progression of thrombosis by thinning the blood.
- ease or ‘decompress’ the congestion of blood in your liver.
- manage your ascites.
- prevent further damage to your liver and allow liver cells to regenerate
- treat the underlying disease that caused the thrombosis in the first place.
Doctors will try to pinpoint the exact area where blood flow obstructed to help them understand how your health may affect. The severity of Budd-Chiari syndrome can depend on where the clot located and the number of veins that are affected.
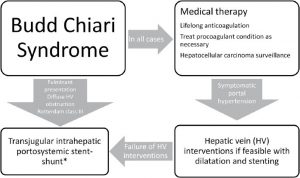
Interventional radiologists
Interventional radiologists will use X-ray techniques known as hepatic angiography or venography to examine arteries. and veins directly to determine the location and severity of a clot. If the inferior vena cava is being examined, an X-ray called inferior cacography used. These procedures involve inserting a thin, flexible tube (catheter) into a blood vessel through an easily accessible vein in the arm, neck, or groin. A dye referred to as a ‘contrast dye’ or ‘contrast medium’, then injected through the catheter to light up the blood vessels to make it easier to see in the X-ray. In some cases, the scan shows that only the end portion of the vein blocked and that much of the vein remains clear. In other cases, the vein more blocked and doctors will need to get to the vein via a tube put into the liver from the tummy.
Venoplasty or angioplasty:
Once the tube gets to the blockage, doctors can remove the clot and open the vein. This is called venoplasty or angioplasty. The vein opened with balloons and the interventional radiologist often decides to place a metal spring (stent) within it to keep it open.
Thrombolysis:
If the clot within the hepatic veins formed recently and difficult to remove, the catheter tube may be left in the hepatic vein for a day or two to allow clot-busting drugs (thrombolysis) to get rid of the clot. When venoplasty/stent succeeds it usually leads to rapid improvement in the patient’s overall condition.
TIPPS (stent in the veins):
In some patients, the blockages are too extensive for venoplasty to work. Doctors will look at which treatments are suitable for the symptoms, depending on how severe they are. When ascites or bleeding varies troublesome, a radiological procedure called TIPSS may offere. This lowers the pressure in the portal vein. In this procedure, a metal or plastic tube (stent) is passed across your liver to make a shunt, or bypass, to make your blood travel straight from the portal vein past the blocked hepatic veins into the inferior vena cava which carries the blood back to the heart. This done using a needle guided by a catheter inserted through a tiny puncture in your neck. This procedure may performed either under general anesthesia or with sedation.

Surgical shunts:
Occasionally another operation may offer which reverses the flow in the portal vein so that it taking blood out of the liver rather than into it. The liver still receives enough blood from the hepatic artery to function adequately. This operation uses a vein from the neck or an artificial graft to make a new connection which allows the blood to escape from the congested liver. Followings shunts can create
Porto-caval shunt
Meso-caval shunt
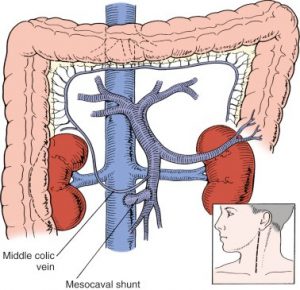
These surgical procedures and TIPSS can effective, however, there a risk they can create an additional problem. The shunts mean that less blood goes through the liver to cleaned of toxins. As a consequence, there a risk these toxins will build up and this can cause a condition called hepatic encephalopathy. The symptoms of this can include mental confusion, tremors, or drowsiness. Hepatic encephalopathy can treated using laxatives such as lactulose, or antibiotics, to help your body remove these toxins. In very few cases the TIPSS stent can altered in size to try and reduce the encephalopathy.
Anticoagulation:
Most experts now recommend that patients with Budd-Chiari syndrome should receive life-long anticoagulation therapy because Budd-Chiari syndrome often means that people’s blood a tendency to clot too readily. Anticoagulation therapy involves taking medicines and being closely monitored with regular blood tests
Treatment of Myeloproliferative Neoplasia (MPN):
In patients with MPN, the hematologist will assess the patient’s disease type and the risk of further thrombosis in order to recommend the appropriate treatment. Assessment includes a molecular test from the blood for acquired mutations, such as JAK2, and a biopsy of the bone marrow. The treatment for MPN usually involves taking drugs long term to control the activity of the bone marrow and blood counts. This type of treatment called cytoreductive therapy and consists of either taking tablets or injections, which require monitoring on a regular basis.
Liver transplantation:
A liver transplant is usually only recommended if other treatments no longer helpful and your life threatened by end-stage liver disease. In Budd-Chiari syndrome, a liver transplant may require when:
- an onset of fulminant Budd-Chiari syndrome causes your liver to fail.
- your liver stops performing all of its functions adequately, a condition called decompensated cirrhosis.
- shunt procedures cannot prevent further deterioration in your condition.
A major operation and if it, not an emergency treatment, you will need to plan it carefully with your medical team, family, and friends. Liver transplants offer a good prospect of a full recovery.
The prognosis (Outlook)
Being diagnosed with Budd-Chiari syndrome can worrying and frightening, as it a serious disease. Diagnosis also gives patients an opportunity to have an effective treatment that can improve their quality of life. Treatments aim to reduce the risk of the disease progressing to a serious outcome and to improve the quality of life. How well you respond to treatment will depend on your age and the severity of the disease at diagnosis. Over 80% of patients do respond well and still alive 10 years after diagnosis. You should speak to your own doctor about your prognosis.

