CANCER OF THE LIVER
Patient Education Material
The Liver
The liver is the largest solid organ in the human body. It lies within the tummy on the right side of the ribs, just below the lungs. The liver has two lobes and is further divided into 8 segments.
The Liver and Bile Duct System
Unlike other organs in the human body, the liver’s blood supply is double by two vessels that supply blood, oxygen, and nutrients. The portal vein brings blood from the digestive system and accounts for 70-80% of the liver’s blood supply. The hepatic artery carries 20-30% of blood to the liver. Liver tumors get to take blood supply from branches of the hepatic artery Hepatocellular Carcinoma (HCC). The liver is your body’s metabolic factory and helps to control more than 500 chemical reactions, including:
- Storing carbohydrates
- Breaking down proteins
- Converting ammonia to urea a substance found in urine
- Using fats to provide energy
- Producing cholesterol which is needed for the production of bile (which in turn helps to digest fats in the food) and hormones.
- Storing minerals and vitamins
- Processing blood (breaking down old red blood cells and producing clotting factors).

Cancer:
The human body is made up of millions of cells. These cells have different shapes and functions in different parts of the human body. The routine wear & tear of the body cells is controlled by a process called the cell cycle. This process strictly regulated by the body’s control mechanisms. In cancers, the cells reproduce in an uncontrolled fashion which can lead to the formation of growth or tumor. The cancer cells develop the ability to invade and destroy surrounding cells by a process called invasion and eventually can spread to the other parts of the body (a process called metastases). Some of the cells that form a lump are malignant (cancerous) others benign (non-cancerous).
The cells which do not spread to other parts of the body (benign tumors) may cause symptoms as they grow by pressing on the surrounding organs. A lump can diagnose as benign or malignant with help of different investigations; such as blood tests, x-rays, ultrasound, and CT scans. Examination of the affected cells under a microscope can confirm the diagnosis of cancer. The special stains & techniques can also help to determine the origin of cancer. This can also tell us whether cancer has started in the area affected (primary) or spread from another part of your body (secondary).
The Liver Cancer:
Cancers in the liver can be either primary (originating in the liver) or secondary (for example, from the intestine). If it starts from liver cells it is called hepatocellular carcinoma or HCC. If it starts from cells of the bile ducts in the liver then it is called cholangiocarcinoma or if starts in the gallbladder, then it is known as gallbladder carcinoma. Cancers in the liver which have spread from another part of the body are usually named after the primary site (for example, liver metastases from a bowel primary).
HCC is the sixth most common cancer in the world. Liver cancer usually develops in a cirrhotic liver, where the cells have been destroyed and replaced by tough scar tissue. Viral infections like hepatitis C (HCV) and hepatitis B (HBV) are the main cause of liver cirrhosis. The other causes include fatty liver disease, auto-immune hepatitis. Liver cancer/HCC is more common in people over 50, and men are slightly more likely to develop it than women.
Due to the high prevalence of HCV and HBV in Pakistan; liver cancer is increasingly being diagnosed in younger patients. Twenty percent of liver cancers are found in a liver that does not have cirrhosis, Liver cancer in infants and children is called hepatoblastoma.
Symptoms of Liver Cancer (HCC):
The general symptoms are non-specific and include weight loss, lethargy/tiredness, loss of appetite, indigestion, and abdominal pain.
Once cancer causes a blockage of the bile ducts symptoms include; pale feces, dark urine, itching, and jaundice. You can experience pain in the upper right side of the tummy and it may spread up to your right shoulder. We may discover HCC as a result of a routine health check where you have had no symptoms at all. Occasionally, we only identify HCC after you have come in as an emergency admission for acute abdominal pain because the tumor has burst. Rarely, cancer causes a blockage of the bile ducts symptoms to include; pale feces, dark urine, itching, and jaundice (yellowness of eyes).
Clinical evaluation by the doctor to look for any signs of chronic liver disease, such as ascites (fluid in your abdomen) and/ or jaundice.
Blood tests:
measure the level of liver enzymes in your blood because your liver may release more if there is a problem.
Check for hepatitis B and hepatitis C
Check for the amount of iron because cancer can cause you to become anemic.
Check for clotting levels because the liver plays a role in blood clotting
Tumor markers in the blood: These are substances normally found in your blood, but if you have cancer they may be high. The tumor marker associated with HCC is called alpha-feta protein (AFP). However, cancer does not always release this protein and there are also certain blood types that do not produce AFP.
Ultrasound scan
CT scan: To get the size, location, and number of cancers in the liver and also helps to plan the best possible treatment
MRI (magnetic resonance imaging): some cancers are more clearly visible on MR scan
PET scan:
occasional done to look for the spread of cancer outside the liver
Angiography: This type of scan is not used often, but can help us take a better look at the blood vessels in and around your liver.
Biopsy:
We can usually identify HCC using a combination of clinical assessment, blood tests, and scans. But sometimes we have to do a biopsy; if the diagnosis is not clear. During a biopsy, a thin needle is inserted into your liver using a scan for guidance. A sample of tissue is taken to examine closely under a microscope.
Treatment of Liver Cancer (HCC):
The aim of the treatment is to treat cancer and any symptoms it may cause. Complete surgical removal of the cancer is the mainstay of liver cancer treatment. The treatment of liver cancer depends on the stage of cancer and may differ from person to person because of:
Location of HCC:
can occur anywhere in the liver. The liver has lots of blood vessels and if cancer developed near one of the two main blood vessels some types of treatment, such as surgery and radio-frequency ablation, may impossible or very high risk. Cancer may affect more than one part of the liver, or it may affect both lobes, which can also restrict the types of treatment.
Size of HCC:
the tumor may grow to a relatively large size before they cause any symptoms, while others may be too small to identify using scans or other tests.
Spread of HCC outside the Liver:
Scans can detect whether cancer has spread to any other part of the body, including lymph nodes. The lymph node system runs throughout the body and if cancer spreads to it this can increase your risk of cancer spreading; further increasing the risk of cancer recurrence after main cancer has been removed.
Age of the patient:
Age can affect how well your body works, however, when deciding on which treatment is the best for each individual, it is important to assess each person’s actual health, rather than expected health for someone of that age.
Associated medical problems:
Are you well despite having another illness or does you have other medical problem limiting your lifestyle or life expectancy? Curable or palliative (may alleviate symptoms) therapies may be offered to you, depending on the factors mentioned above. The clinical team caring for you will discuss, with you, the different treatments and therapies available. They will assist and support you in making decisions and choices about what is right for you. If your other medical illness is a chronic liver disease, we may still be able to offer you treatment that cures you, such as liver transplantation. This depends on the size and position of your cancer.
Some patients can be offered treatments that potentially completely curative; others can be candidates for treatments that may shrink the tumor or slow its growth. Some patients can be offered only palliative care which aims to control their symptoms. The clinical team caring for you will discuss the different treatments and therapies available. The team will give you the help and support you need to decide what is right for you.
What are the treatment options available:
There are different treatments and therapies available;
Liver Transplantation:
Liver transplantation is a potential cure for you. Not all patients are suitable candidates for liver transplantation. There are certain agreed international guidelines that are followed to decide whether you are a potential candidate for a liver transplant. These rules consider how large the tumor is and whether it has spread outside the liver or invaded into the blood vessels. If you are considered an as suitable transplant candidate then you will undergo a full assessment. A big advantage of a liver transplant is that it not only potentially cures liver cancer, it also cures the underlying liver disease.

Liver Resection:
Liver resection involves the complete removal of the tumor. This treatment can offer a potential cure in few patients. To have a resection, the tumor needs to be restricted to one lobe of the liver and there should be no sign of it spreading to blood vessels or other organs. In addition, the baseline liver function needs to be good.

Ablation Therapies:
radio-frequency ablation (RFA), microwave ablation, cryoablation, and percutaneous ethanol injection (PEI). These treatments involve the local destruction of cancer. The most commonly used local ablative therapies are radio-frequency ablation (RFA) and percutaneous ethanol injection (injecting pure alcohol into your tumor). These can also be used as a ‘bridge treatment’ while you await liver transplantation or as a treatment prior to liver resection surgery.
With RFA a thin needle is inserted into the tumor using an ultrasound or CT scan to guide us and then use radio-frequency or microwaves to damage the tumor tissue. You have this treatment under local or general anesthesia.

With PEI, we inject a sterile and highly concentrated alcohol solution directly into the tumor to produce a similar effect to RFA.
Both techniques can control tumors long-term if they are small in size and number. We can also use them together with other treatments as part of an overall plan to manage your condition.
Trans-arterial chemo-embolisation (TACE):
TACE (or chemoembolization) is generally used if the tumor is too advanced to consider a treatment that could potentially cure you. It may also be used as a ‘bridging treatment’ while you await liver transplantation or as a treatment prior to liver resection surgery.
In TACE a thin tube called a catheter is passed via a blood vessel in your groin to the blood vessels supplying the liver. A chemotherapy drug is injected directly into the tumor and block the blood vessel supplying it. The drug and the ischemia (blocking the blood supply to the tumor) damage the tumor tissue. TACE will not cure you but aims to shrink your tumor and stop it from getting bigger.
Trans-Arterial Embolization (TAE):
TAE is exactly the same as TACE and with the same aim, but without the chemotherapy drug. It will offer to you if it is not appropriate to use a chemotherapy drug.
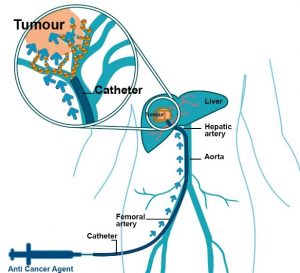
Trans-Arterial Radioembolization (TARE):
TARE is exactly the same as TACE and with the same aim, but with a radioactive isotope (small radiation-emitting particle) instead of a chemotherapy drug. It will be offered to the patients if it is not appropriate to use a chemotherapy drug.
Drug treatment (Sorafenib):
This is an oral medicine. It has been shown to prolong the lives of some patients with liver cancer in whom the liver cancer is advanced to cure. It is generally considered if the tumor is too advanced for treatments that could potentially cure you and TACE is either ineffective or not possible for technical reasons. Sometimes this drug is used as an adjunct treatment to TACE
Currently, there are multiple other drugs being tested in research (trials). The medical community is constantly researching new ways to treat cancer. Clinical trials are a way of assessing and/or comparing new treatments and new combinations of treatment. If we think you may benefit from any trial treatment we will explain what it involves when we offer it to you.
Palliative care:
If after a detailed discussion of the treatment options you and your family decide rather not to receive any active treatment for your condition, or we feel that active treatment would not help you; the team will refer you for palliative care (supportive care to alleviate symptoms, not a curative treatment) near your home. Supportive care can also be offered to you if you are undergoing treatment such as chemotherapy, which is not expected to offer you a cure.

