CANCER OF THE PANCREAS
Patient Education Material
What is Pancreas?
Pancreas:
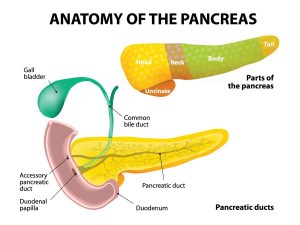
The pancreas is a gland that lies across the back of your upper abdomen, behind the stomach and guts (intestines), and in front of the spine, and just above the level of your belly button (umbilicus). Its shape is like a cylinder and is about 15cm long and 3cm wide. The pancreas has two main functions.
-
Exocrine function:
- It produces a fluid called “pancreatic juice” that flows through a small tube in the center of the pancreas called the pancreatic duct into your small intestine (duodenum). Pancreatic juice helps to digest the food so that the proteins, fats, and carbohydrates can be digested and then absorbed into the bloodstream and used for energy for other body functions.
-
Endocrine function:
- Groups of special cells called ‘Islets of Langerhans’ are scattered throughout the pancreas. These cells make the hormones insulin and glucagon. The hormones are passed (secreted) directly into the bloodstream to control the blood sugar level in the body.
The bile duct carries bile from the liver and gallbladder. This joins the pancreatic duct just before it opens into the duodenum. Bile passes into the duodenum and helps to digest food.

Cancer:
The human body made up of millions of cells. These cells have different shapes and functions in different parts of the human body. The routine wear & tear of the body cells controlled by a process called the cell cycle. This process strictly regulated by the body’s control mechanisms. In cancers, the cells reproduce in an uncontrolled fashion which can lead to the formation of growth or tumor. The cancer cells develop the ability to invade and destroy surrounding cells by a process called invasion and eventually can spread to the other parts of the body (a process called metastases). Some of the cells that form a lump are malignant (cancerous) others are benign (non-cancerous).
More about Cancer:
The cells which do not spread to other parts of the body (benign tumors) may cause symptoms as they grow by pressing on the surrounding organs. A lump diagnosed as benign or malignant with help of different investigations; such as blood tests, x-rays, ultrasound, and CT scans. Examination of the affected cells under a microscope can confirm the diagnosis of cancer. The special stains & techniques can also help to determine the origin of cancer.
Cancer of the pancreas means a malignant tumor of the pancreas. This may occur anywhere along the length of the pancreas.
Pancreatic Cancer:
Pancreatic cancer is uncommon cancer and not much known about its cause despite so much research. However, we do know that smoking increases the risk. A history of pancreatic inflammatory disease (chronic pancreatitis) and pancreatic stone disease is associated with an increased risk of developing pancreatic cancer. There can also be a family history of pancreatic cancer. The pancreatic cancer usually a slow-growing cancer and can spread to other parts of the body in the later stages of the disease. Its incidence is about 80-130 per million population in the western world. In Pakistan, its incidence is on the lower side and it’s around 30 per million population per year. Usually, it is more common in men and affects people over 50 years of age; however recently young patients in their 4th decade of life are being diagnosed with bile duct cancer in Pakistan.
Symptoms of Pancreatic Cancer:
symptoms of pancreatic cancer a “silent” disease which means symptoms may not occur. The general symptoms are non-specific and include weight loss, lethargy/tiredness, loss of appetite, indigestion, and abdominal pain. You may experience pain in the upper right side of the abdomen which may radiate through to the back.
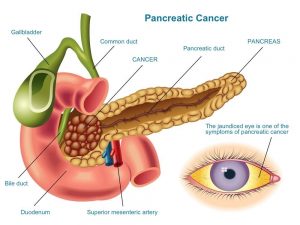
Once cancer causes a blockage of the bile ducts symptoms include pale feces, dark urine, itching, and jaundice (yellowing of the skin).
How to treat Pancreatic Cancer:
Clinical evaluation by the doctor to look for the presence of jaundice (yellowness of skin and eyes) or presence of scar marks (due to itching) and presence of any lumps in the tummy.
Blood tests including LFT’s (bilirubin level in your blood will high due to the blockage of the bile duct).
Hemoglobin (Hb level) can below
Tumor markers. These are substances normally seen in the blood, however, in people with cancer, they may high. In pancreatic cancer, the tumor marker associated with it is Ca19.9.
Ultrasound scan
CT scan
MRI (magnetic resonance imaging)
Endoscopic Retrograde Cholangio-Pancreatography (ERCP)
Endoscopic ultrasound (EUS)
You may undergo one or more of the scans in order to help identify the tumor and assess your suitability for the various treatments.
Histology/cytology All of the previously mentioned tests may lead the doctor to diagnose bile duct cancer. However, the only definite way to confirm this diagnosis is to examine some of the abnormal tissue (cancer cells) under a microscope. Some cells taken during the ERCP procedure (these called brushings). These cells taken to the laboratory for cytology examination. However, the results of cytology do not always produce a diagnosis and may give a negative result, despite cancer existing. If a larger sample of tissue required we may perform a biopsy. This when a needle passed through your skin, into the affected area. If your doctor planning to treat your cancer with surgery, you may not undergo a biopsy, as tissue confirmation can obtained after the operation, by the laboratory.
Treatment:
Complete surgical removal of cancer the mainstay of pancreatic cancer treatment. The aim of the treatment is to treat cancer and any symptoms it may cause. Treatment of pancreatic cancer depends on the stage of cancer and may differ from person to person because of:
Location of the tumor:
Pancreatic cancer can occur anywhere within the pancreas. As the pancreas sitting on the major blood vessels, cancer may develop near one of these vessels making surgery impossible or very high risk.
Size of the Tumor:
Pancreatic cancers may grow to a relatively large size before they cause any symptoms. While some may cause symptoms but may too small to identify on scanning or other tests.
The spread of Cancer:
CT scans can detect whether cancer spread to any other part of the body – including the lymph glands. As the lymph system runs throughout the body, cancer that may have spread to the lymph system can increase the risk of further cancer spread (metastases) or increase the risk of cancer recurrence where the main cancer already surgically removed.
Age of the patient:
Age can affect how well your body works, however, when deciding on which treatment the best for each individual, it is important to assess each person’s actual health, rather than expected health for someone of that age.
Associated medical problems:
Are you well despite having another illness or does you have other medical problem limiting your lifestyle or life expectancy? Curable or palliative (may alleviate symptoms) therapies offered to you, depending on the factors mentioned above. The clinical team caring for you will discuss, with you, the different treatments and therapies available. They will assist and support you in making decisions and choices about what is right for you.
Surgery:
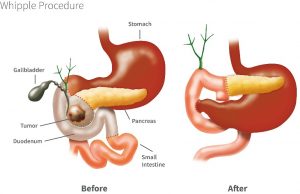
Surgery may be offered as a potentially curable or palliative treatment. At present complete surgical removal of cancer offers the only possible cure. The commonest surgical operation performed to remove pancreatic cancer a pancreaticoduodenectomy, often called a Whipple’s procedure. This operation takes 5-7 hours and involves removing most, if not all of the pancreas, the gall bladder, the bile duct, and part of the small intestine. Nearby lymph nodes may also removed as a part of the radical operation.
Palliative surgery:
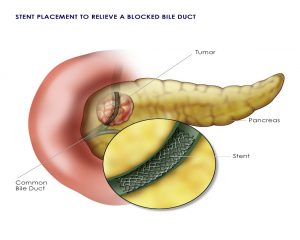
offered if the obstruction of the bile ducts or obstruction to the stomach by cancer cannot be alleviated by any other means, for example, stent insertion (a fine plastic or metal tube).
Stenting:
The insertion of a plastic or metal tube into the blocked bile duct, in order to keep it open, called stenting. It helps to restore the flow of bile into the intestine and can alleviate jaundice. The stent inserted by a procedure called Endoscopic Retrograde Cholangio-Pancreatogram (ERCP), and it’s done by gastroenterologists/ hepatologists. This is the preferred way of stent placement as it is more convenient for the patient. In the case of failed ERCP, the other way to insert the stent called Percutaneous Transhepatic CholangioPancreatogram (PTC), and this procedure done by specialist doctors called interventional radiologists. PTC only used for a very tiny proportion of the stents placed for patients with pancreatic cancer.
If the cancer-causing a narrowing of the small intestine (duodenum) this can cause problems with your ability to eat and drink and leads to vomiting after meals. A stent, larger than that used for the bile ducts, used and inserted into the duodenum to allow you to eat and drink, without nausea and/or vomiting.
Chemotherapy:
The treatment of cancer with drugs is called chemotherapy). This treatment may be offered as a palliative treatment, where surgery not possible, or as an add-on to surgical treatment. The aim of the palliative it to potentially slow down and/or shrink cancer. As an “add-on” (adjuvant) treatment, it is offered to treat any cancer that may remain after surgery. Each dose of chemotherapy (single or combination) is called a cycle, each cycle is usually separated by 2-3 weeks of a recovery period. This allows your body to receive the treatment, react/respond, and recover.
More about Chemotherapy
Very occasionally patients may be offered chemotherapy, sometimes with radiotherapy, to shrink their tumor with a view to later performing surgery; this called neo-adjuvant chemotherapy or chemo-radiotherapy. It can be very difficult to predict how someone, or cancer, will respond to chemotherapy. However, in some people, even if a response is not achieved, they may find it alleviates their symptoms and may prolong their life expectancy.
Unfortunately, with pancreatic cancer, it is very difficult to predict whether it will respond to chemotherapy. However, in some people, even if a response is not achieved, they may find it can alleviate their symptoms and may prolong their life expectancy.
Palliative care:
If after a detailed discussion of the treatment options you and your family decide rather not receive any active treatment for your condition, or we feel that active treatment would not help you; the team will refer you for palliative care (supportive care to alleviate symptoms, not a curative treatment) near your home. Supportive palliative care can also be offered to you if you undergoing treatment such as chemotherapy, which not expected to offer you a cure.

