CHRONIC PANCREATITIS IN ADULTS
Patient Education Material
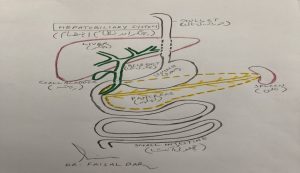
Pancreas:
The pancreas is a gland that lies across the back of your upper abdomen, behind the stomach and guts (intestines) and in front of the spine, and just above the level of your belly button (umbilicus). Its shape like a cylinder and about 15cm long and 3cm wide. Chronic Pancreatitis has two main functions
- Exocrine function: It produces a fluid called “pancreatic juice” that flows through a small tube in the center of the pancreas called the pancreatic duct into your small intestine (duodenum). Pancreatic juice helps to digest the food so that the proteins, fats, and carbohydrates can be digested and then absorbed into the bloodstream and used for energy for other body functions.
- Endocrine function: Groups of special cells called ‘Islets of Langerhans’ are scattered throughout the pancreas. These cells make the hormones insulin and glucagon. The hormones are passed (secreted) directly into the bloodstream to control the blood sugar level in the body.
The bile duct carries bile from the liver and gallbladder. This joins the pancreatic duct just before it opens into the duodenum. Bile passes into the duodenum and helps to digest food.
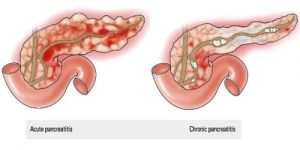
Pancreatitis means inflammation of the pancreas. There are two types.
Acute pancreatitis:
when the inflammation develops quickly, over a few days or so. It usually goes away completely and leaves no permanent damage to the pancreas. Sometimes it serious.
Chronic pancreatitis:
The inflammation persistent. The inflammation tends to less intense than acute pancreatitis but as it ongoing it can cause scarring and damage. About 4 in 100 people across the world at any one time have chronic pancreatitis
It not known how many people in Pakistan have this condition, but it thought to have increased considerably over the years. It more common in men than in women.
Causes of Chronic Pancreatitis
Alcohol – The common cause in the western world. Men aged 40-50 are the most common group of people affected. In most cases, the person drinking heavily for 10 years or more before symptoms first begin.
Smoking – Recently found to linked to chronic pancreatitis.
Genetic conditions – their some rare genetic conditions that can lead to chronic pancreatitis developing. Cystic fibrosis one cause. Genetic means you born with it and it passed through families through special codes inside cells called genes.
Autoimmune conditions –
your own immune system attacks the pancreas. This can be associated with other autoimmune diseases – for example, Sjörgren’s syndrome and primary biliary cirrhosis.
Other causes – are uncommon. They include abnormalities of the pancreas such as narrowing of the pancreatic duct (due to various reasons) and conditions inherited from one of your parents (hereditary).
Malnutrition – and eating lots of cassava a cause in some countries.
Unknown – in some cases, no cause identified. No cause found in around 2 out of 10 cases of chronic pancreatitis.
Note:
gallstones, which a common cause of acute pancreatitis, do not cause chronic pancreatitis unless the little tube which attached the gallbladder to the liver (the bile duct) damaged by a stone or by infection.
What happens in Chronic Pancreatitis?
A persistent inflammation develops in the pancreas. The reason why alcohol or other factors trigger this inflammation not clear, although in some people it thought to relate to their genes. Over time the inflammation causes scarring and damage to parts of the pancreas. This can then lead to not enough chemicals (enzymes) and insulin being made. A lack of enzymes causes poor digestion of food (malabsorption). A lack of insulin causes diabetes. Over time clumps of calcium deposited and can form stones in the pancreas.
More about Chronic Pancreatic:
Calcium stones and/or scarring of the pancreatic ducts may block the flow of enzymes along the pancreatic ducts. Chronic pancreatitis often becomes worse with time. The time from the initial triggering of inflammation to damage, scarring, calcium stones, and then to developing digestion problems or diabetes, often several years. However, many months or years of this process can go on before any symptoms first noticed.

Symptoms of Chronic Pancreatitis
The symptoms can vary between cases. The most common symptoms include:
Tummy (abdominal) pain – just below the ribs is common. The pain typically felt spreading through to the back. It tends to be persistent and may be partly eased by leaning forward. It mild at first but can become severe. Eating often makes the pain worse. This may lead to your eating less and then losing weight. The pain intermittent so not present all the time.
Note: around 1 person in 5 with chronic pancreatitis any abdominal pain. Poor digestion (malabsorption) – occurs if not enough enzymes are made by the damaged pancreas. In particular, the digestion of fats and certain vitamins is affected. Undigested fat from the diet may remain in the gut and be passed with stools (feces). This causes pale, smelly, loose stools that difficult to flush away (steatorrhoea). Weight loss can also occur if food not fully digested.
Diabetes –
occurs in about 1 in 3 cases. This occurs when the pancreas cannot make sufficient insulin. Symptoms usually include excess thirst, passing large amounts of urine, and further weight loss unless diabetes treated. However, chronic pancreatitis actually an uncommon cause of diabetes.
Feeling sick (nausea) – and generally feeling unwell may also occur.
Chronic Pancreatitis diagnosed:
Unfortunately, there currently no single test for chronic pancreatitis. Diagnosing chronic pancreatitis in its early stages is often difficult. Many pancreatic cells damaged before abnormalities show up on tests, X-rays, or scans. The number of enzymes made by the pancreas and the number of insulin-producing cells can become quite low before any symptoms of poor digestion or diabetes develop. Once the damage and scarring to the pancreas more severe, or when calcium stones start to form, then the damaged pancreas can detected by X-rays or scans. However, by this time the malabsorption or symptoms of diabetes may have already developed.
Tests done usually include:
- Blood tests to check your blood count, kidney, and liver function.
- Blood tested for diabetes.
- Your doctor may also request a sample of your feces (poo, stools or motions) for testing.
- An X-ray or CT scan of your tummy (abdomen) may be performed.
- A cholangiogram is a test that produces a picture of the bile ducts. This often done using an MRI scan.
- Looking at the pancreas with a telescope put down into your stomach. Occasionally, the dye squirted up the tube leading to the pancreas (the pancreatic duct) to obtain a clearer picture of what going on.
What complications can develop?
Most people with chronic pancreatitis do not have complications. However, the following may occur:
- Pseudocyst – develops in about 1 in 4 people with chronic pancreatitis. This when pancreatic fluid, rich in chemicals (enzymes), collects into a cyst due to a blocked tube that leads to the pancreas (the pancreatic duct). These can swell to various sizes. They may cause symptoms such as worsening pain, feeling sick, and vomiting. Sometimes they go away without treatment. Sometimes they need to drain or surgically removed.
- Ascites – sometimes occurs. This fluid collects in the tummy (abdominal) cavity between the organs and guts (intestines).
- Blockage of the bile duct – an uncommon complication. This causes jaundice as bile cannot get into the gut and leaks into the bloodstream. This makes your skin look yellow.
- Cancer of the pancreas – more common than average in people with chronic pancreatitis. The risk increases in smokers and with increasing age
- Rare complications – include blockage of the gut, bleeding or blood clot (thrombosis) in blood vessels near to the pancreas.
It fairly common to feel low when you have chronic pancreatitis, especially if you in pain. Some people even become depressed, which can respond well to treatment. It important to talk to your doctor about any symptoms of depression you may have.
-
Stop drinking alcohol for good
- this is the most essential part of treatment. You should not drink alcohol even if it is not the cause of your chronic pancreatitis.
- Painkillers – usually needed to ease the pain. Controlling the pain sometimes becomes quite difficult and referral to a pain clinic may be needed. Apart from painkillers, other techniques to block the pain may be considered, such as nerve blocks to the pancreas.
- Enzyme replacement medication – may be needed if the low level of chemicals (enzymes) causes poor digestion of food and steatorrhoea. Capsules containing artificial enzymes are taken with meals.
- Restricting fat in the diet – may be advised if steatorrhoea is bad.
- Insulin – if diabetes develops then insulin injections will be needed to control the blood sugar level.
- Vitamins – may need to be taken.
- Do not smoke – to minimize the risk of pancreatic cancer developing.
If you have autoimmune pancreatitis then you may be given a course of steroid tablets.
Surgery:
Most people with chronic pancreatitis do not need surgery but an operation sometimes needed. The common reason for surgery for persistent bad pain that not helped by painkillers or other methods. Improvement in pain occurs in about 7 in 10 patients who have surgery. The operation usually involves removing part of the pancreas. There are different techniques that remove different amounts of the pancreas. The one chosen depends on the severity of your condition, whether the pancreatic duct blocked, and also on various other factors.
Other operations may be advised in some cases – for example, removal of a large calcium stone that is blocking the main pancreatic duct. Another procedure that may help in some people is to ‘stretch’ wide a narrowed pancreatic duct to allow better drainage of pancreatic enzymes.
More about surgery:
Surgery may also be needed if a complication develops. For example, if a blocked bile duct or pseudocyst develops. If the pain is persistent you may be offered a procedure to block the nerve supply to the area. Examples of treatments that involve this approach are coeliac plexus block and spinal cord stimulation. If you need surgery, then your surgeon will be able to discuss with you in detail the type of operation you need.

The Prognosis for Chronic Pancreatitis:
If alcohol is the cause of chronic pancreatitis then other alcohol-related illnesses also commonly develop. If you continue to drink alcohol and pancreatitis becomes severe then life expectancy typically reduced by 10-20 years. This due to complications of pancreatitis or to other alcohol-related illnesses. If you stop drinking alcohol completely in the early stages of the condition, the outlook better. The outlook for other less common and causes of chronic pancreatitis depends on the cause and severity of the condition.

