GALLSTONES
Patient Education Material
Gallstones
Gallstones stone-like objects that form in the gallbladder or bile ducts. Gallstones can be tiny (the size of a grain of sand), or maybe as large as a golf ball. Depending on the symptoms, people who have gallstones may not need treatment, or they may need to take medication or have surgery to remove their gallbladder. If the stones are in the bile ducts, they usually need to be removed by endoscopy.

Gallbladder
The gallbladder is an organ that resembles a small pear. It located under the liver on the right side of the abdomen. The function of the gallbladder to store and dispense bile, a fluid produced by the liver and helps digest fats in the foods you eat. Bile is made up of several substances, including bilirubin and cholesterol.

connected to the liver and the intestine by a group of ducts, including the hepatic duct, the cystic duct, and the common bile duct. When you eat, gallbladder sends bile through the common bile duct into the intestine to help you digest food, particularly fatty foods.
The following have an increased risk of developing Gallstones:
- People over the age of 40.
- People who have a family history of gallstones (relatives who the disease).
- People who overweight or
- People who lose a great deal of weight in a short period of time.
- People who have
- People with Crohn’s disease.
- People whose diet is high in fat and cholesterol.
- People who take drugs that lower cholesterol.
- American Indians and people of Mexican descent.
There are 2 types of Gallstones:
pigment stones (made up of bilirubin) and cholesterol stones (made up of cholesterol). Most gallstones are cholesterol stones.
Cholesterol gallstones can form when there too much cholesterol or bilirubin in the bile. Gallstones can also develop if the gallbladder does not completely empty itself of bile.
Pigment gallstones may form in people who certain conditions, such as cirrhosis of the liver or blood disorders.
Symptoms of Gallstones
In many cases, people who have gallstones do not any symptoms. These gallstones are known as “silent stones.”
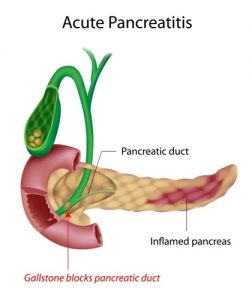
The main symptom of gallstones pain, which can last from several minutes to several hours. Pain can occur when gallstones move from the gallbladder into one of the ducts (the hepatic duct, the cystic duct, and the common bile duct). Gallstones that migrate can cause conditions such as acute cholecystitis (inflammation of the gallbladder), cholangitis (infection and inflammation of the bile ducts), and pancreatitis (inflammation of the pancreas).
The pain located in the upper part of the abdomen, between the shoulder blades, or under the right shoulder.
Other symptoms of gallstones include:
- Sweating
- Vomiting
- Fever
- A yellow tint to the skin (jaundice)
Ultrasound abdomen:
a procedure that transmits high-frequency sound waves through body tissues. The echoes recorded and transformed into video or photographic images of the internal structures of the body.
Other tests that may help in the diagnosis of gallstones include the following:
Computed tomography (CAT scan)
Endoscopic retrograde cholangiopancreatography (ERCP):
In this test, an endoscope—a flexible tube with a light and a camera attached—inserted into the patient’s mouth, down the throat, and into the stomach and small intestine. A dye is injected to allow the bile ducts to stand out. If their gallstones in the bile duct, they removed by the endoscope.
Magnetic resonance cholangiopancreatography (MRCP):
In MRCP, the bile ducts examined with magnetic resonance imaging (MRI), a test that uses a large magnet, radio waves, and a computer to produce very clear images of parts of the body. Unlike ERCP, MRCP can only diagnose gallstones; it cannot be used to treat gallstones.
Endoscopic ultrasound (EUS):
This procedure combines endoscopy with ultrasound. In EUS, a small ultrasound transducer is installed on the tip of an endoscope and inserted into the patient’s mouth. Because the EUS transducer can get close to the gallbladder and bile ducts, the images obtained with EUS more accurate and detailed than images provided by traditional ultrasound.
How are gallstones treated?
In most cases, if you have gallstones in the gallbladder but no symptoms (silent stones), you probably do not need treatment.
If you have symptoms such as pain, you will probably need to be treated. The treatment that used most often for gallstones is surgery to remove the gallbladder, which is known as a cholecystectomy. In the vast majority (90%) of cases, this surgery is performed laparoscopically.
Laparoscopic cholecystectomy
Laparoscopic cholecystectomy knew as a “minimally invasive” procedure because it uses several small incisions instead of one large one. A laparoscope, a narrow tube with a camera, inserted through one incision. The camera allows your doctor to see your gallbladder on a TV screen. Your gallbladder then removed through another small incision.
In most cases, if you have gallstones in the gallbladder but no symptoms (silent stones), you probably do not need treatment.
If you have symptoms such as pain, you will probably need to be treated. The treatment that used most often for gallstones surgery to remove the gallbladder, which known as a cholecystectomy. In the vast majority (90%) of cases, this surgery performed laparoscopically.
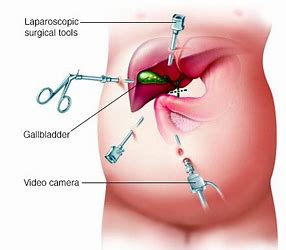
More about Laparoscopic cholecystectomy
If the patient has certain complications associated with gallstones – such as inflammation, infection, major scarring from previous surgery, a bleeding disorder, or a condition that would make it difficult to see through the laparoscope – the surgeon may have to remove the gallbladder with an open cholecystectomy through an incision in the abdomen. This procedure requires a longer hospital stay (3-5 days).
If their gallstones in the bile duct, they need to be removed in most cases even if you do not have any symptoms. This is done most commonly with the endoscopic retrograde cholangiopancreatography (ERCP) procedure.
You don’t need a gallbladder in order to digest food properly. If your gallbladder removed, bile will flow directly from your liver through the hepatic duct and the common bile duct to the small intestine. After the surgery, you will probably have to go to the bathroom more frequently, and you may have softer stools for a short time.
Non-surgical treatment
If a patient unable to undergo surgery, the doctor can prescribe certain drugs to dissolve the gallstones. The drugs are made from bile acid and are used to treat cholesterol stones only.
Complications of Gallstones:
Gallstones can block the ducts and hinder the flow of bile from the liver or gallbladder to the intestine. This blockage can cause bloating, nausea, vomiting, and pain in your abdomen, shoulder, back, or chest.
also, cause the gallbladder or bile ducts to become infected. A blockage in the common bile duct can cause jaundice (yellowing of your skin or eyes) or can irritate the pancreas.
If you have any further questions or worries please feel free to ask the staff on your ward, your surgical team or your clinical nurse specialist.
Patient Help Line (PHL)
Patient Help Line (PHL) a service that offers support, information and assistance to patients, relatives and visitors. They can also provide help and advice if you have a concern.
Transplant coordinator:
Mr. Touseef Ahmed 0333-1027353
Transplant Coordinator: (for post-transplant follow up patients):
M. Zaheen Hashmi 0333-1027354
Hepatobiliary & Pancreatic Surgery Services:
Muhammad Asif 0341-0543883
24 Hours Patients emergency Helpline: 0333-1027356
Email: info@faisaldar.com
Counselling service: The counselling service offers free and confidential sessions to our inpatients, outpatients, their relatives and friends. If you would like to meet with one our counsellors you can contact us on 0333-1027356
Transplant coordinator:
Mr. Touseef Ahmed 0333-1027353
Transplant Coordinator: (for post-transplant follow up patients):
M. Zaheen Hashmi 0333-1027354
Hepatobiliary & Pancreatic Surgery Services:
Muhammad Asif 0341-0543883
24 Hours Patients emergency Helpline: 0333-1027356

