INFORMATION FOR LIVING LIVER DONORS
Patient Education Material
liver
A piece of liver removed from a living donor and transplanted into a recipient to replace their own diseased liver.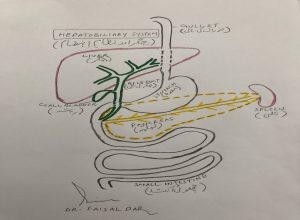
The liver a large organ and is considered to be the “metabolic factory of the human body. Naturally liver is a” paired organ” composed of the right and left lobes joined together. With advanced surgical techniques, the liver can be divided into two separate and functionally independent units and this is the basis for living donor liver transplantation.

Living liver donation because the liver can regenerate. Regeneration of the liver happens over a period of about six to eight weeks. The transplanted liver will also grow or shrink to an appropriate size for the recipient.
The first living donor liver transplant in 1988 was performed in Brazil of a child who received part of an adult liver. In 1994 the first Adult to Adult Living Liver Donor Transplant performed in Japan. Thousands of living donor liver transplants been performed so far across the globe. The living donor liver transplantation an established form of treatment for patients with end-stage liver disease.
Anyone who is genetically related to the recipient, for example, parent, spouse, brother or sister be considered as a possible donor.
- Adults aged between 18 and 50 years
- You should not be overweight
- You should not have a major medical illness
- You should not have a major psychiatric illness
- You should be able to understand all the potential complications and risks of surgery
- You should have a compatible blood group with the recipient
- You should be genetically or legally related to the recipient
Confidentiality
Donors will be given information regarding the recipients of liver disease and the possibility of recurrence of the original disease. Recipients will not be given information regarding the donor’s test results or the reason why a donor is not suitable.
If you are considering donating part of your liver to a relative or friend it is essential that:
- Your liver is suitable for the recipient
- The risk to your own health is minimal
- No financial or other pressure is being put on you to donate
- Reason for donation must be voluntary and altruistic
You should contact the transplant coordinator to note your interest in becoming a donor. After some initial information you will be given an information folder. We will also request that you have your blood group checked before your first clinic appointment.
It is not possible to be a donor if you are not related to the recipient. The Human Organ Tissue Authority protocols and guidelines have to be met. “It is a criminal offence to carry out a transplant operation between two living people if the conditions of the HOTA Act are not met. This includes valid consent being given by the donor and the recipient”
Living donor liver transplantation is now an established form of treatment for children and adults with end stage liver disease with 85-90% of those who receive a liver transplant from a living donor alive at one year after their transplant. This is comparable with the patients who receive a transplant from cadaveric donors.
There are a number of potential advantages of having a living donor; however the most important is that the recipient does not have to wait many months for a cadaveric liver due to the scarcity of cadaveric donors in Pakistan. If a recipient has a suitable living donor they may avoid becoming much sicker during a stressful waiting period. For a number of patients their health may deteriorate over time and they may become unsuitable for transplant. For example patients with hepatocellular carcinoma may have disease progression during the waiting time.
Theoretically there is less risk of rejection due to the genetic similarity in the donor to recipient graft. Surgery can be electively planned and the potential recipient optimised to the best of health where a potential living donor is available. The quality of a living donor liver may be better than that of a cadaveric liver, as the living donor will have undergone a strict assessment prior to being accepted as a donor. Preservation time for a living donor is much shorter than the preservation time for a cadaveric donor or non-heart-beating donor; this also contributes to a better quality liver.
More than 500 vital functions have been identified with the liver. Some of the better-known functions include:
- Regulating blood clotting
- Production of bile, which helps break down fatty food
- Removal of toxins and drugs from the blood
- Manufacture certain blood proteins
- Convert and store excess glucose to use for energy
- Stores iron.
When the liver has broken down harmful substances, they are excreted in the bile into feces or filtered via the blood and kidneys and leave the body in the form of urine.
Donor Assessment
What is the purpose of the assessment?
- To ensure that you have no medical or surgical contraindications for donation
- To ensure you have no psychiatric conditions that would exclude you from becoming a donor
- To provide you and your family with all the necessary education and information including costs prior to you deciding to go ahead with the surgery
- To ensure you are undertaking this decision on your own free will without any pressure or financial gain
The recipient must satisfy current criteria for liver transplantation prior to the commencement of a living donor assessment. The evaluation ensures that the donor’s liver is normal and of adequate size and that the donor does not have any medical or psychiatric illness that would increase the risk of the procedure. The transplant team have to be sure that the donation is voluntary and that there is no undue pressure on the donor to undergo living donation.
The evaluation will involve a series of blood and radiological investigations, reviews by separate medical and surgical consultants, psychiatric assessment. The Living Donor Transplant Coordinator will be responsible for coordinating the assessment and counseling the donor.
This is then sent to the Human Organ Transplant Authority (HOTA) and a decision regarding permission to proceed to donation is received. The HOTA have a maximum of 5 days to return a decision on an Adult donation. Additional documentation required for the Human Organ Transplant Authority includes copies of national ID cards/passports, family registration certificate (FRC), photographs of the recipient and donor, and birth certificates where available.
No, the liver transplant team will perform all the examinations for the living donor. We will coordinate appointments and try to minimize the number of visits to the hospital for assessment.
Testing the blood group is a simple blood test. You must be the same blood type as your recipient or blood group O.
If you are a suitable blood type and are wishing to be considered as a living liver donor for your relative, you can contact the transplant coordinator on the telephone number and discuss living liver donation or schedule an appointment to meet in the hospital. Registration details can be taken over the phone and a hospital record created for you.
An appointment with the transplant coordinator and Transplant Surgeon, Dr. Faisal Dar will be arranged. The transplant coordinator will perform a health screen and provide an opportunity to ask questions. The transplant coordinator will inform you of the potential risks and benefits of living donation and what the evaluation process involves. The potential risks of donation and the possible outcomes of the donor evaluation will be discussed. The potential donor can stop the evaluation or withdraw from the process at any time right up to the donor surgery.
The surgeon will take a brief medical and surgical history and examine your abdomen. The surgeon will discuss living donor liver transplantation with you, including the potential risks and the statistics on the procedure at our hospital and worldwide. The surgeon will discuss the chances of a donation being successful in each individual case.
The transplant coordinator will get you to sign a consent form if you are still intending to be assessed as a living liver donor. The followings tests will be done at this stage:
Blood tests:
- To check the function of your liver
- To check the ability of your blood to clot
- To see if you are anemic (low hemoglobin)
- To assess the function of your kidneys
- To check the level of oxygen in your blood
- For viruses – including Hepatitis B, Hepatitis C, Cytomegalovirus (CMV) and the HIV virus.
Chest x-ray: to ensure you have no lung problems
ECG / echocardiogram: to assess the function of your heart
Pulmonary function tests: breathing tests which provide a detailed assessment of your lungs
Scans: ultrasound of the abdomen will be requested. The blood tests will be reviewed and then the second step of the assessment will be booked.
The second step of evaluation.
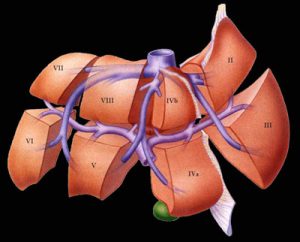
This will include computerized tomography (CT) of the liver to enable calculation of the volumes of the right and left lobes. Magnetic resonance imaging (MRI) will be needed to look at the liver structure. These tests will provide information on the supply of blood to and away from the liver.

A Consultant Hepatologist will interview you. Other tests and consultations may be required depending on your results. For example, if your pro-coagulation screen (clotting profile) is abnormal you may be required to see a Consultant Hematologist for specialist advice regarding the suitability to donate, and any special precautions that may be advisable. A second example may be if you have been found to have hypertension (high blood pressure) a Consultant Cardiologist may be requested to review the donor for expert advice. The Consultant Hepatologist will make the decision if a liver biopsy is necessary.
The transplant coordinator will provide further counseling surrounding the donation surgery. Again the risks associated with the living donation will be discussed. Potential complications that the recipient may encounter including rejection, primary non-function, biliary complications, vascular complications, and the long-term side effects of immunosuppression will also be discussed. The possible after-effects following donation and the recommended convalescence period and long-term complications for the donor are discussed. The consultant anesthetist will discuss the anesthetic and pain relief postoperatively.
You are advised not to eat for 4 hours prior to your abdominal ultrasound. You are allowed to drink water or black coffee but not to take any milk or dairy based products. You are not requested to fast prior to your CT or for your MRI. It is ideal that you have a fasting lipid profile, so that the Cholesterol level is accurate.
It is helpful to have immediate family or next of kin with you to some of the appointments so they can participate in the evaluation process. It will provide them with a better understanding of the process. It also provides an opportunity for them to ask questions. The Independent Assessor is required to see both the donor and the recipient together if possible, as part of the assessment. The independent assessor will in time need to establish that there is no pressure or coercion on the donor from the family or others, and that donation is voluntary and that the donor has the capacity to understand what they are undertaking. The independent assessor will also need to establish the recipient’s willingness to accept the living donation from the donor.
After the medical assessment is complete we can inform you of your suitability as a living donor. We cannot confirm until the final confirmation by the Human Tissue Authority return a permission number or reference to the particular application for permission to proceed to living liver donation.
If you require time for contemplation or time to get your social supports in place, the transplant team will arrange the planned date for donation around your request. You may find you need time to digest all the information to consider the risks and benefits.
Once the tests are complete and the Human Tissue Authority is in agreement with the planned donation the transplant team will meet and review your results. The Hepatologist, Surgeon, Anaesthetist, Transplant coordinator, Social Worker and other specialists involved in your evaluation will have a multidisciplinary meeting.
This will be a joint decision between the transplant team, you and the recipient. The date will be arranged and the recipient’s team will optimize the recipients’ health for this date. Resources have to be fully available for the living donor surgery to proceed to maintain optimal safety.
As a donor you are volunteering to donate part of your liver in attempt to help the recipient. Before making this gift, it is important that you understand the likelihood is that you will save that life, but this can never be taken for granted and some recipients may have complications of the surgery and may even die. Some diseases such as hepatitis C and cancer of the liver can recur after transplant. For patients whose liver disease was caused by excessive alcohol we make certain they fully understand the implications of returning to drinking alcohol and a support system will be offered to them to assist them to remain free from alcohol but we can’t promise their compliance. The surgeon will have explained to you expected outcome from the donation. It is important that you understand and respect the confidential nature of these discussions and maintain the recipient’s privacy under these circumstances. The recipient will be aware of the need to maintain confidentiality regarding your medical details as well.
Yes, you are completely free to withdraw from the procedure at any stage. Also the transplant team can stop the assessment process at any stage. You will be given a full explanation on this. The reason for withdrawal will be kept confidential and only the transplant team will be aware of it.
Nurses: Will prepare you for your procedures and care for you after your operation.
Transplant Coordinator: Support you throughout the process from beginning to end, arranges all your investigations. Provides you with all the education you require.
Fellow hepatology: Will be responsible for your complete assessment, and will take care of you before and after surgery.
Consultant Transplant Surgeon: Will ensure you and your family is fully aware of all the risks and benefits of surgery. He will perform the operation.
Donor Advocate: Usually a physician outside of the transplant team, who will help you understand the process, procedure, and risks and benefits of live organ donation and to protect and promote your interests and well-being as a donor. You can opt to withdraw at any time during the assessment process. The reasons for withdrawal will be kept confidential.
Consultant Physician: Will ensure you have no medical contra-indications to the liver surgery.
Consultant Anesthetist: Will discuss the anesthetic and post-operative pain control with you.
Consultant Psychiatrist: Will ensure you have no psychiatric contra-indications to the surgery and you fully understand the implications of donating part of your liver. He will confirm that you are doing this voluntarily without any undue pressure.
Social Worker: Will discuss the reasons for offering to donate part of your liver. He/she will assist you in becoming socially and emotionally prepared to undergo a major operation. He/she will give you advice regarding benefits and other practical issues.
Physiotherapist: Will ensure you are aware of the importance of early physiotherapy following the operation.
The amount of liver required will depend on the size and the sickness of the recipient. For an adult-to-adult living donor transplant, up to 70% of the donor’s liver may be removed. The liver is divided into a left and a right lobe. The anatomical division between the lobes enables the surgeon to divide the liver into two distinct parts. Both parts of the liver can function independently of each other. The right lobe is approximately 60-70% of the liver and the left lobe approximately 30-40% of the liver. The donor gallbladder is removed. The recipient gallbladder is also removed at the time of transplant. For an adult to child living donation the left lateral segment of the liver is removed (about 20% of the liver).
The donor operation usually starts at 08.00 am and the recipient surgery overlaps with the donor surgery. The approximate start time of the recipient surgery is 09.30hrs. The recipient transplanting surgeon will check with the donor lead surgeon if the liver is satisfactory and what the expected time for the liver coming out will be. Adult to adult living donor donation take place utilizing two theatres. Both the donor and recipient always go to intensive care following surgery. Two surgical teams are separately responsible for donor and recipient respectively.
As with any operation involving a general anesthetic there are possible complications. While these complications are rare, the risk does exist and we will discuss them in more detail with you during the assessment. Generally 10- 20% of donors will experience some form of complication. This means there is a one in 5 chance that the donor will experience problems after the donation.
- Death – the risks of death are very real and must be considered seriously.
According to results reported from centers around the world the risk of death for the live liver donor is between 0.5% for adult to adult right lobe donation and 1 in 500 for left lateral segment donation for an adult to child donation.
- Need for urgent liver transplant – If the remainder of your liver does not function properly you may require an urgent liver transplant to save your life. Every effort will be made during assessment that such an eventuality does not arise.
The most common complications include;
- Bile leak – from the cut surface of the liver, mostly settles with non-operative treatment.
- Bleeding – the liver has a rich blood supply.
- Clots in legs or lungs – the same risk as with any other major abdominal surgery.
- Heart attack – Before surgery, you will be checked thoroughly for heart disease.
- Infection – at the wound site or pneumonia.
These usually resolve after a couple of weeks. There is a risk that pain management may be difficult and you could experience severe pain. You may experience nausea or itching or dizziness from the strong painkillers. While the risks are rare the however exist and will be discussed with you in detail by the transplant coordinator during your assessment. You will be likely to notice a loss of sensation on your lower abdominal wall but this will return over time.
It is unlikely that you will require a blood transfusion during the living donor surgery. However, we prepare blood for transfusion in case it should be necessary. We use a ‘cell saver’ device and your own blood can be given back. This avoids the risks associated with receiving transfusion blood.
Yes. If you are going to be a liver donor, stop drinking. If you have a history of heavy alcohol use you should tell your physician. Alcohol use may not preclude you from being a donor but you may need to undergo a liver biopsy to be sure your liver has not been damaged.
Yes, we strongly advise you to stop smoking; even if you are a light smoker, as your risks of complications including chest infection and delayed wound healing will be significantly higher if you continue to smoke. Smoking may not preclude you from being a donor but you should stop it at least 4 weeks before surgery.
No. Do not stop any prescription medication unless advised to stop by a Doctor. Avoid Aspirin or non-steroidal medication such as brufen/ neurofen for seven days before a biopsy or surgery. These medications affect the ability of the blood to clot and put you at higher risk of bleeding complications. You may use Paracetamol.
Women taking the contraceptive pill or pills for hormone replacement therapy will be advised to stop taking them because of the increased risk of blood clots during recovery from surgery.
You could expect to be off work for 6 to 8 weeks. As people recover at different rates and varying degrees of fatigue and pain it may take up to 12 weeks to feel fully recovered. Ideally we prefer that you are in a position both financially and from a job security perspective to be able to take 12 weeks to recover if you need that much time.
The incision is large; it will go across your abdomen and may have a T incision going upward towards the ribs.
Yes you will have a scar. The wound heals quickly. The scar will heal over time. If you have the complication of a wound infection this may impact on your scar and it could be wider than just a fine scar. Occasionally, people develop excessive healing tissue. This is over growing or over healing of the skin and it results in a raised scar. This can be corrected by plastic surgery at a later date.
Yes. You will have significant pain after this surgery but this will be treated to make you comfortable. You will be offered an epidural for pain relief. If there are difficulties with the epidural the pain team will organize an alternative pain control supply. It is important to control the pain as much as possible to enable you to breathe well and to begin to move comfortably as soon as possible after the surgery. You will need to be monitored closely as most pain medication is broken down by the liver and now you will have up to 60% less liver than before so you may be more sensitive to the drugs being administered. Most pain medication will make you drowsy and affect your breathing and bowel function. We try to get the balance right to ensure your safety and comfort.
You need to be comfortable enough to be able to do your breathing exercises, coughing, limb exercises and walking. You will receive pain medication on discharge to ensure your comfort at getting back to the daily activities of living you previously performed without any discomfort.
As soon as you feel comfortable. The decision will depend on how you are feeling.
It is advisable to wait at least 3 to 6 months to allow the abdominal wall optimal chance to recover and heal.
It is advisable to wait for 3 months before restarting hormone therapy.
The liver begins to re-grow almost immediately. The first two weeks after surgery probably sees the greatest surge in re-growth. By 3 months the liver is probably back to near its original size for both donor and recipient.
No. You can only donate part of your liver once.
We advise you not to drive for 6 weeks following your surgery. You must be physically and mentally strong, with normal reflexes and not experiencing any abdominal discomfort before you decide to drive. You should not be using medication with codeine in as these can affect your mental alertness.
As soon as possible, you need to start taking long deep slow breaths once you wake up from the anesthesia. You need to make a cough to ensure you are getting air into the bottom on your lungs. This will help to avoid chest infection.
You should begin flexing and relaxing your limbs also.
Move your feet in circular directions and bring your legs up and down the bed. Avoid friction to your heels, do not damage your skin. It is recommended that you try and do a few of these exercises hourly when awake. After 24 hours you will be assisted to sit to the edge of the bed with the physiotherapist and slowly transferred to a chair taking few steps initially and gradually increasing the amount of walking. You are encouraged to push yourself a little more each day. Early mobilization helps to reduce the risk of blood clots and chest infection. You are encouraged to continue a programme of daily exercise of walking and breathing and coughing. Remember the goal is to return to normal within 8 weeks.
You will need to avoid any heavy lifting for the 3 months until your abdomen has completely healed. You should not lift any weights greater than 10 kg. After 6 to 8 weeks you may begin to return to your normal activities if you are not having any complications. Swimming, jogging, aerobics, cycling etc. should not be a problem, just begin slowly and build up gradually. Heavy lifting should not be attempted for 3 months.
Wait for 4 weeks and preferably 8 to 12 weeks after your surgery. If you are wishing to return to home, you may be able to go 3 to 4 weeks after the surgery depending on your recovery. If you develop any possible complications you will be required to report back for assessment and treatment.
No. It may not take place when it is planned due the lack of availability of ICU beds, and the need to reschedule the living donation. If the recipients’ condition was to deteriorate the date may be brought forward. If they become un-transplantable it may change the plan. If the recipient had cancer there may be a request for an exploratory laparotomy prior to proceeding with the donation and if these were to show disease spread outside of the liver, the donation would not proceed. If a cadaveric donor became available the transplant team may proceed to use this organ and the living donor would not be used.
The donor will be in hospital for approximately 7 -8days.
Both the donor and the recipient will go to the Intensive Care following surgery. They will be in separate cubicles.
As soon as your intestines start to work again after surgery, you will be able to eat and drink. You will be able to wet your mouth and use oral swabs once you are awake. . You will be started on sips of fluid the next morning and progress slowly to free fluids and light diet as you tolerate same.
Yes. You will have a naso-gastric tube in your nose draining your stomach. This will help to resolve any nausea as the bag drains the content of your stomach. You will have a central line in your neck into a large vein. This will be used to give you intravenous fluids to keep you hydrated and also to give you medicines. You will have a catheter in your bladder draining your urinary output to see how your kidneys are working during and after the surgery. You will have a small drain in the right side monitoring any potential ooze or leak form the cut edge of the liver. You will have a very fine catheter in your spine if you have an epidural for pain management. The tubes and drains will be removed over the next 4 to 5 days. The tube in the nose is usually removed on day 1 following surgery. The epidural is usually removed day 4 and so is the urinary cather. The abdominal drain is usually removed about day 4 if it is clear and not draining very much. The neckline is removed about day 4 depending on the intravenous support being required. Once the intravenous fluids stop the donor is encouraged to drink up to 2 Liters of fluid and to resume diet as tolerated.
Yes, you will need to be monitored closely at first to ensure everything is OK. You need to have bloods checked and an ultrasound to ensure there is no abdominal collection. You will be required to come to clinic at 1 week, 4 weeks and 6 months and then annually pending the findings.
If you are from overseas we request you stay in the Pakistan for 4 to 6 weeks after donation. We do request you contact the transplant coordinator if you are having any difficulty or complication related to the surgery. It is important you have family or social support following your discharge form hospital.
Yes, you will be expected to require painkillers for a few days following discharge. If you should develop any complications you may require medications for it. We do not foresee that you would require any long-term medication following surgery.
No. Extremely unlikely. You can expect to feel tired and weak, you will be more likely to need company and a helping hand. Your friends and family members will be more helpful with food shopping, cooking and generally helping out. Someone to accompany you to your follow up appointments would be helpful.
You will have a dissolvable stitch in your wound which will not require removal. The only stitch to be removed will be the one securing the abdominal drain when that is removed.
The evaluation for donors is very thorough. Once the evaluation is complete and a decision to proceed is agreed there is little additional testing. You will have baseline bloods repeated the evening prior to the surgery and an ECG. You will be invited to see the intensive care and liver wards prior to your admission.
No, eat and drink as normal. You need to fast for 6 hours prior to the planned operating theatre start time. If you take any regular medications you will be advised about these the night before surgery. You should not drink alcohol for 3 months preceding surgery. Remember if you use oral contraceptive therapy it must be discontinued 3 months before surgery. Do not take Aspirin or non-steroidal drugs like Neurofen within seven days of your surgery.
Yes, you and your recipient will be admitted to hospital at approximately 15.00hrs the day before your surgery. You will have been reviewed by the anesthetist during the evaluation. The consultant surgeon will see you and complete a second consent form with you for the surgery. Remember you can change your mind up-to the time you are going to surgery.
Bring minimal belongings, no valuables, and no jewelry. Bring basic toiletry and ask your family to hold it for you.
The time expected to lapse from the commencement of the donor evaluation to the setting of a potential date for surgery is approximately 2 weeks. In emergency situations the assessment can be complete in much less time.

