NEUROLYSIS AND PLEXUS INFILTRATIONS
Patient Education Material
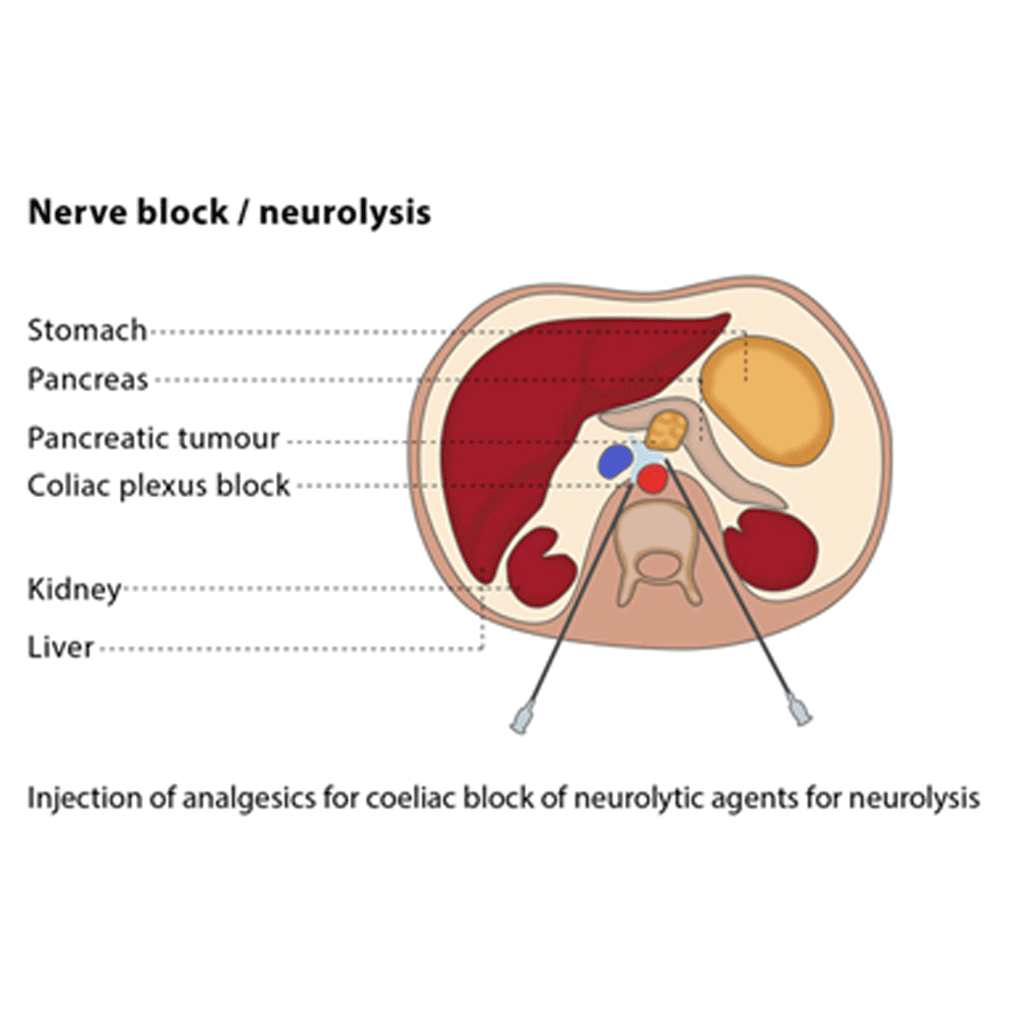
Neurolysis is the deliberate destruction of a nerve or a network of interlacing nerves (plexus) with the aim of providing permanent relief from pain by interrupting the transmission of pain signals in the nerves.
Nerve block refers to temporarily blocking the function of a nerve by injecting painkillers into the area around the affected nerve, thus blocking the transmission of pain signals. This temporarily disables the nerve without causing permanent damage.
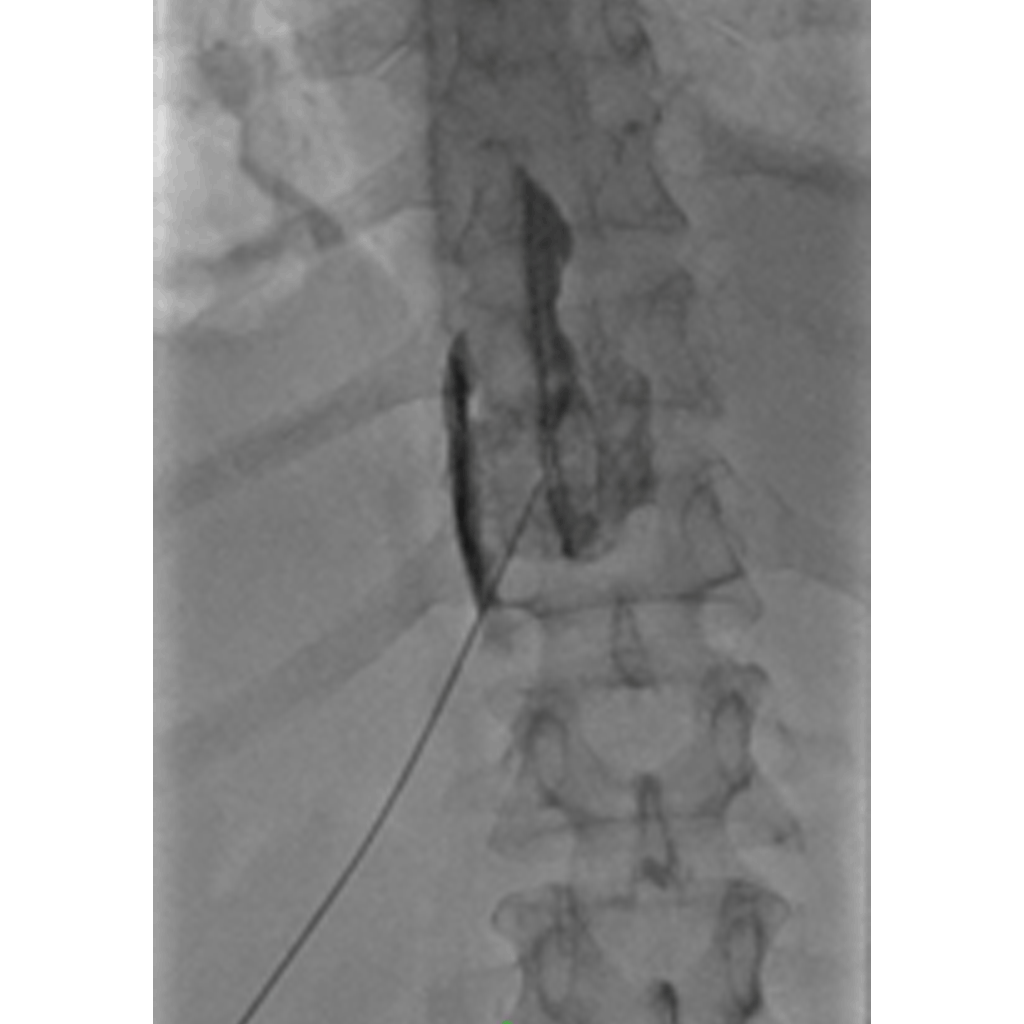
If you are undergoing neurolysis, there are a number of techniques that the interventional radiologist may use. The most common method of causing permanent nerve destruction is the injection of a chemical such as alcohol. Alternately, the interventional radiologist may choose to use ablation techniques to destroy the nerves. In these cases, the interventional radiologist will insert a needle or a thermal probe into the area so it is in contact with the nerve or the plexus.
If you are having a nerve block, the interventional radiologist will use a single thin needle to inject anaesthetics (sometimes mixed with anti-inflammatory drugs) into the area around the nerves responsible for pain.
Because these procedures are carried out under image guidance, the interventional radiologist can target the precise area, which reduces the risk of complications when targeting deeply situated nerves.
Neurolysis can be used to treat severe diseases including chronic pain. It is most often used as a pain control technique for cancer patients but can also be used to treat other conditions causing chronic pain which appear to have no cure or no clear cause.
There are some minor side effects associated with the procedure, depending on the nerve targeted. For example, neurolysis in the abdominal splanchnic nerves often causes orthostatic hypotension, also known as ‘head rush’, when a person’s blood pressure falls when standing or stretching. Severe complications for a nerve block or neurolysis are rare. However, as is the case with all procedures near the spine, there is an exceptional risk of paralysis of the area supplied by the nerve or elsewhere.
- Akural E, Ojala RO, Järvimäki V, Kariniemi J, Tervonen OA, Blanco Sequeiros R. MR-guided neurolytic celiac plexus ablation: an evaluation of effect and injection spread pattern in cancer patients with celiac tumor infiltration. Cardiovasc Intervent Radiol. 2013 Apr; 36(2):472-8.
- Masala S, Crusco S, Meschini A, Taglieri A, Calabria E, Simonetti G. Piriformis syndrome: long-term follow-up in patients treated with percutaneous injection of anesthetic and corticosteroid under CT guidance. Cardiovasc Intervent Radiol. 2012 Apr; 35(2):375-82.
- Yilmaz S, Ceken K, Alimoglu E, Sindel T. US-guided femoral and sciatic nerve blocks for analgesia during endovenous laser ablation. Cardiovasc Intervent Radiol. 2013 Feb; 36(1):150-7.
Kindly contact:
- One PKLI Avenue, DHA, Phase-6, Lahore, Pakistan.
- info@pkli.org.pk
- +92 42 111 117 554