PANCREATIC SURGERY FOR CANCER
Y
Patient Education Material
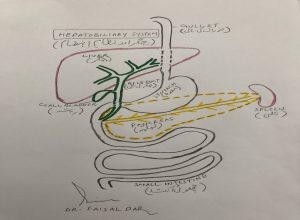
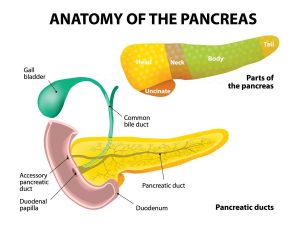
Pancreas:
The pancreas a gland that lies across the back of your upper abdomen, behind the stomach and guts (intestines) and in front of the spine, and just above the level of your belly button (umbilicus). Its shape like a cylinder and about 15cm long and 3cm wide. The pancreas has two main functions.
-
Exocrine function:
- It produces a fluid called “pancreatic juice” that flows through a small tube in the center of the pancreas called the pancreatic duct into your small intestine (duodenum). Pancreatic juice helps to digest the food so that the proteins, fats, and carbohydrates can digeste and then absorbed into the bloodstream and used for energy for other body functions.
-
Endocrine function:
- Groups of special cells called ‘Islets of Langerhans’ are scattered throughout the pancreas. These cells make the hormones insulin and glucagon. The hormones are passed (secreted) directly into the bloodstream to control the blood sugar level in the body.
The bile duct carries bile from the liver and gallbladder. This joins the pancreatic duct just before it opens into the duodenum. Bile passes into the duodenum and helps to digest food.
Why do pancreatic operation:
patients with pancreatic cancer need this operation because it the most effective way of removing the tumor in the pancreas.
Before any surgery patient’s clinical condition and CT scans review to get an idea of how the tumor in the pancreas can be best removed. All the tests and scans will be reviewed by the multidisciplinary team (MDT). The team will recommend the treatment it considers to be the best for you. This recommendation discussed with you before a final decision made.
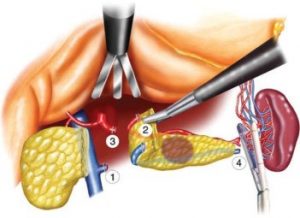
Pancreatic resection
Pancreatic resection a surgical operation to remove the tumor from the pancreas. This is a complex operation because of where the pancreas sits in the body and its connections to other digestive organs. The pancreas is joined to both the intestine and the bile duct, so during the operation, depending on the extent of your disease and the type of pancreatic resection being performed, these parts of the body may also have to be removed and reconnected.
Different types of pancreatic resection:
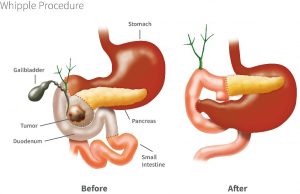
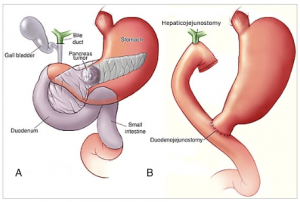
Pancreaticoduodenectomy (Whipple’s procedure):
This operation done when the tumor is located in the head of the pancreas, the lower end of the bile duct, or in the duodenum. This the most commonly performed pancreatic resection, first described by an American surgeon named Dr. A.O. Whipple. More commonly this operation is called “Whipple’s procedure”.
It involves the removal of the head of the pancreas (30%-40% of the gland), the duodenum (early part of the small intestine), part of the bile duct, and gallbladder. There a small chance that you may become diabetic following this surgery, or if you already diabetic, it may affect your diabetic control.
Distal pancreatectomy:
If the tumor in the pancreas in the body or tail of the pancreas you will able to undergo a distal pancreatectomy – the removal of the tail and body of the pancreas along with the spleen. The spleen needs to be removed because it closely applied to the tail of the pancreas.
This operation can also perform laparoscopically (keyhole surgery) and this something that will be offered to you if indicated.
If you already a diabetic, you may have a period of variable diabetes control post-operatively.
Total pancreatectomy (complete removal of the pancreas):
This involves the removal of the whole of the pancreas, the duodenum, distal extra-hepatic bile ducts, gallbladder, and spleen. Following a total pancreatectomy, all patients will become diabetic and will require insulin.
Benefits of Pancreatic:
The intended benefit is that the operation will extend your life expectancy. Currently, surgery the only treatment that can potentially provide a chance of cure for your cancer. Patients who able to undergo resection for their pancreatic cancer survive longer than patients who cannot.
While pancreatic resection is carried out with the hope of curing you of your cancer, there is a risk of the tumor coming back after the operation and you will have regular follow-up scans at your local hospital to monitor this. The likelihood of recurrence depends on the type of tumor you have and how far it has spread at the time of surgery.
After surgery;
After surgery, the resection specimen reviewed and this will be helpful in deciding whether any additional treatment (chemotherapy) require. Discussions on any further treatment will take place with you while you in hospital and at your outpatient appointment.
Please tell us if you have any allergies. Please tell us if you on any anti-coagulation drugs (anti-platelet/ blood-thinning) including warfarin, aspirin, heparin, clopidogrel.
Pancreatic surgery
Pancreatic surgery a complex major surgery and the chance of dying as a result of the operation in the region of 2% – 3% although your individual risk calculated based on your clinical condition and will be discussed with you prior to the final decision to operate.
Some risks are common to all operations, such as chest infection and blood clots forming in the leg veins (DVT) or in the lungs (pulmonary embolus). However, there also specific risks associated with pancreatic surgery.
Bleeding:
One of the major risks is bleeding. You can lose blood during the operation and, if required, this will be replaced with blood transfusions; the risk of requiring a transfusion is 1 in 10 or 10%. Occasionally bleeding can occur after the operation and a further operation may be necessary to stop this. Transfusion itself carries some risks and would not be given except when absolutely necessary. If you have any objections to receiving blood or blood products (such as platelets) it essential that you inform your surgeon and/or anesthetist before your operation.
Anastomotic leak:
The reconnections (or anastomoses) that create during the operation can sometimes leak. If this happens further drains (to drain the leaking fluid to the outside) may be necessary. The leakage rate approximately 8-10% of patients. If there is a serious leak of pancreatic fluid you may need to be fed intravenously for 10 -20days. It is also possible that you may also have to return to the theatre for further surgery, though this is rarely necessary. If a leak occurs this will almost certainly extend your hospital stay.
Infection:
This may involve the wound, the drain sites, or the inner organs. Antibiotics will given to you at the time of surgery to try to prevent infections. If there a lot of infection in the bile duct you could develop sepsis (serious infection of the body) after the procedure. Patients who have stents inserted in their bile ducts before surgery is at increased risk of developing infections. However, the antibiotics you will be given should limit this risk.
Advanced disease:
sometimes it is not clear from the tests you have had prior to surgery whether the tumor is removable. The scans can under-stage cancer in 15-20% of the cases. So; it may not be until you are actually on the operating table that it is discovered that the tumor cannot be removed. In our experience, this occurs in 3-5% of patients taken to theatre for pancreatic resection surgery.
Change in diagnosis following surgery:
sometimes the final histology may not prove the presence of cancer, despite the evidence on all the pre-operative investigations. This is a rare occurrence (1-3%).
Splenectomy:
when the spleen has to be removed as part of the operation (as a planned part of a total or distal pancreatectomy, but a risk with any pancreatic surgery) this will be discussed with you before and after your operation. The spleen helps you fight infection and if your spleen removed then you will be given vaccinations. In addition, you will need to take antibiotics regularly (usually penicillin or Amoxycillin) for about 2-5 years after surgery.
Delayed stomach emptying:
This can be a temporary problem that may lead to nausea, vomiting, and loss of appetite. This can be helped with anti-sickness medications and/or nasogastric feeding (via a fine tube inserted up the nose, down the back of the throat into the stomach).
Digestive enzyme and hormone production (including insulin):
Removal of part, or all, of the pancreas, can permanently affect the body’s ability to produce certain products that help to digest food and regulate blood sugar levels. If this occurs you will still be able to lead a normal life provided you take regular enzyme supplements and/or insulin injections. Should you require insulin you will be provided with the support of diabetic specialists, who will help explain the monitoring of blood sugars and the safe administration of insulin.
Everything will be done to try to minimize all of the risks described above.
Alternatives to the pancreatic reaction:
Treatment options depend on the stage of the disease, your age and your fitness to undergo major surgery. Surgical removal of cancer offers the only chance for cure. However, only a small proportion of patients (15%-25%) suitable for surgical resection. After your surgery, depending on the stage of the disease and the outcome of your operation, you may also need chemotherapy.
All the patients who not suitable for surgery, or who choose not to have surgery, may have their jaundice relieved by inserting a tube through the tumor into the bile duct during a procedure called ERCP. This is done without an open operation through a flexible telescope passed into the mouth down the throat and into the stomach and small intestine.
Alternatively the stent can be placed through a Percutaneous Transhepatic Cholangio-gram (PTC). This performed by an interventional radiologist and the stent is inserted percutaneously (through the skin) directly into the liver.
Chemotherapy:
The treatment of cancer with drugs is called chemotherapy). This treatment may be offered as a palliative treatment, where surgery not possible, or as an add-on to surgical treatment. The aim of the palliative it to potentially slow down and/or shrink the cancer. As an “add-on” (adjuvant) treatment, it offered to treat any cancer that may remain after surgery. Each dose of chemotherapy (single or combination) called a cycle, each cycle usually separated by 2-3 weeks of a recovery period. This allows your body to receive the treatment, react/respond and recover.
Unfortunately, with pancreatic cancer, it is very difficult to predict whether it will respond to chemotherapy. However, in some people, even if a response is not achieved, they may find it can alleviate their symptoms and may prolong their life expectancy.
Palliative care:
If after a detailed discussion of the treatment options you and your family decide rather not to receive any active treatment for your condition, or we feel that active treatment would not help you the team will refer you for palliative care (supportive care to alleviate symptoms, not a curative treatment) near your home. Supportive care can also be offered to you if you undergoing treatment such as chemotherapy, which not expected to offer you a cure.
what happens before the operation:
Once surgery agreed with you as the favored option, you will be asked to attend a pre-assessment clinic to assess your fitness for surgery and answer questions. This usually takes half a day and you will be given the opportunity to discuss details of the operation. The pre-assessment nurse and or the anaesthetist will explain the anaesthetic process and discuss the postoperative pain relief options. This usually in the form of epidural analgesia where a small tube inserted in your back to deliver the pain-relieving drugs. Alternatively, a patient-controlled analgesia pump (PCA) will be offered. A PCA allows you to control your own dosage of pain relief, delivered through a drip in your arm, by pressing a small button.
Please use this opportunity to ask the surgeons, nurses or anaesthetists any questions that you have.
The day before the operation, you must not eat or drink anything after midnight as your stomach needs to be as empty as possible for the general anaesthetic you will be given for this operation. This may be given to you when you are in the operating theatre itself, so don’t worry if you are still awake when you are first taken into the theatre.
Consent:
We must by law obtain your written consent to any operation, and some other procedures, beforehand. Staff will explain all the risks, benefits and alternatives before they ask you to sign a consent form. If you unsure about any aspect of the treatment proposed, please do not hesitate to speak with a senior member of staff again.
During the operation, the surgeon will make quite a large cut (incision) across the abdomen. He/she will then check that everything appears to be as expected from CT scans. The part of your pancreas containing the tumor will be isolated. Once the diseased part of the pancreas removed then the other organs will all be reconnected. Connecting the parts back together takes time and complex work.
Once completed, everything checked and the incision closed by several layers of stitching.
Every patient and their surgery is different, so it is impossible to predict exactly how long a particular operation will take, but most pancreatic operations take about six hours to complete.
Pancreatic resection a major operation and you will usually have to stay in the Intensive Care Unit for a short while afterward (usually 24 – 48 hours). This allows the team to closely monitor your progress and recovery. When you’re ready we will transfer you to the ward.
Wounds and drains:
The cut in your skin usually stitched up with dissolvable stitches, so there no need for stitches to be removed. The surgeon will place drains in your abdomen to remove fluids from the operation site. These removed approximately four-five days after the operation.
Circulation:
The nurse will need to check your blood pressure and pulse regularly – initially every hour, then every two to four hours. You will have a small tube in one of your arteries to measure your blood pressure.
Breathing:
You will need to wear an oxygen mask for the first 24 – 48 hours following your operation. This helps with your breathing and recovery. In rare cases, you may still require help from a breathing machine when you leave the theatre. However, in most cases, the tube in your throat will be removed immediately after surgery.
The physiotherapist will see you every day during your stay in the ward and encourage you to practice deep breathing exercises. This is important as it will help prevent you from developing a chest infection.
Eating and drinking:
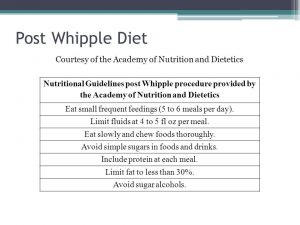
You will not be allowed to eat or drink for up to 3-4 days following your operation. To help stop you from being sick we may place a tube from your nose to your stomach. You will have a drip in a vein in your neck and your arm to provide essential fluid while you cannot drink.
When you feeling better you will be asked to start drinking and eating again by taking sips of water and then gradually building up to a normal diet over the course of a few days. By this time the drip in your neck or arm, and the tube in your nose will be removed.
The pancreas plays an important role in controlling how sugar stored in your body. For the first 48 hours, we will need to check your blood sugar at least every six hours to ensure your pancreas working normally. This involves pricking your finger with a small needle and squeezing a small sample of blood on to a sugar sensor stick. A lot of people will require insulin treatment, at least in the short term.
Passing urine: You will have a tube in your bladder (catheter) draining the urine into a bag, which the nurse will use to measure to monitor your progress.
Pain relief: You will have a pump to control your pain. This will either be an epidural (which runs through a tube in your back) or a PCA (patient controlled analgesia) pump, which connects to a small tube under the skin in your arm. You will be taught how to use this before you have your operation.
Pressure areas:
It is important while you in bed to change position regularly (at least every two hours) so that you can relieve the pressure on your bottom and heels. The nurses will help you to do this.
Getting moving again:
You will be encouraged to get up and about the morning after your operation. The sooner this is done and the more you mobilize, the less likely it that complications will occur. The nursing staff and physiotherapists will help you. You will also have a pair of white (TED) stockings on, as this helps to improve the circulation in your legs and prevent blood clots from forming. Please bring slippers with you to wear over the TED stockings to reduce the risk of you slipping when mobilizing post-operatively.
Physiotherapy:
After your operation, you will be seen by the physiotherapist on the ward to check your chest and help you to begin mobilizing again. Any general anesthetic has an effect on the natural function of your lungs and your physiotherapist will help you to counteract this by teaching you breathing exercises and assisting you to cough effectively. Sitting out in a chair and walking around at an early stage very important for your digestive system and for your circulation and chest, so don’t be surprised if you encouraged to get out of bed on the day after your operation.
You will be “attached” to a variety of tubes (one or more wound drains, a drip, a catheter, and some form of pain relief) but your physiotherapist or the nursing staff will be able to help you with these and you will only be mobilizing with their assistance in the early postoperative stages.
Washing:
Initially, you may feel too tired or weak to be able to walk to the bathroom so the nursing staff can help you to wash.
Medication:
Please bring your normal medication with you when you come into the hospital. You should continue to take your usual medication and this will be prescribed for you (on your medication chart) and dispensed by the nursing staff. In addition, you will be given a small injection twice daily of heparin to prevent you from getting blood clots in your legs. You may also be given antibiotics to help prevent infection.
Do:
- try and sit out of bed as soon as you encouraged to do so.
- the breathing exercises you are taught several times a day.
- let the nursing staff know if you are in pain.
For home
You will be able to go home within 8-12 days after your operation. However, you may need to stay longer if there have been complications that require additional treatment.
By the time you go home, you should be able to manage independently – although you will not feel completely back to your ‘old self’ and should take things slowly. The following information gives you some advice and simple exercises to continue with at home to aid your recovery.
Returning to work:
If you planning to return to work, try to pace yourself and take regular breaks if you feeling tired. Again this depends on the type of work you do and your hospital doctors will be able to answer any more specific questions regarding returning to work.
what should I do at home?
Following your surgery, it may take several weeks to regain your previous level of fitness. Walking is one of the most effective (and easily available) forms of exercise to help your recovery. There no correct distance to be walking, everyone will be different. Aim to slightly increase the distance you cover each day, but don’t exhaust yourself. As long as you can still comfortably hold a conversation whilst walking you will be maintaining a sensible pace. If you are too breathless to talk, stop and rest!
You can then progress to other forms of cardiovascular exercise e.g. gentle cycling, as you feel able. Returning to swimming or the gym will depend on your wound healing, so ask your doctors for more specific information regarding this prior to discharge. However, as a general rule, you should be able to return to active sport after three months.
POST PANCREATIC SURGERY
Do:
- Check your wound daily. If it is hot, red or oozing, contact your doctor as you may have an infection.
- Eat a well-balanced, nutritious diet.
- You can have a shower or bath when the wound is healed with no open areas
- See your doctor if you are worried about your progress.
- Attend all outpatient appointments.
- Follow a regular routine of abdominal and postural exercises once home
- Check with your doctors before swimming or training at the gym
- Discuss your return to work with your doctors
Don’t:
- Expect to feel 100% for several weeks after surgery
- Do too much too soon. Learn to pace yourself
- Use perfumed soap, talc or body lotions on your wounds until they are completely healed.
- Lift anything heavy – including heavy shopping bags or do housework such as hovering for at least 6 weeks after surgery.
- Return to playing the sport for at least three months
- Hesitate to ask questions if you are unsure or worried
In the 6 weeks after surgery, if you develop: rectal bleeding, find blood in your stools or vomit blood, immediately report to us. These symptoms can be indicative of a rare, but life-threatening post-operative complication.
Post-operative exercises to do at home
Lie on your back with knees bent. Squeeze your buttocks together and lift your bottom off the floor. Return to starting position. Repeat 5 times.
Lie on your back with knees bent. Tighten your stomach muscles and push the small of your back against the floor. Hold for 5 seconds and then relax. Repeat 5 times.
Lie on your back with knees together and bent. Tighten your stomach muscles and push the small of your back against the floor. Slowly roll your knees from side to side keeping your back in contact with the floor. Repeat 10 times.
Exercises to improve posture
Because you will tend to be very aware of your wound, it is not unusual for you to hunch over, leading to a stiff back and a tight scar. Once your drains are removed, the following exercises should help to stretch your stomach and back (your wound and stitches will be fine!).
Exercises to strengthen stomach muscles Due to the nature of your operation, your stomach muscles will be weak postoperatively. These muscles act as a ‘corset’, supporting your back and helping with your posture. The following exercises will help strengthen these muscles. You should aim to do each set of exercises once a day.
Stand with your back against a wall. Push gently back into the wall so that your shoulders and the back of your head are in contact with it. Hold for five seconds. Repeat 5 times.
Sit on a chair and fold your arms across your chest. Turn your upper body to look over your shoulder as far as comfortable. Repeat the exercise on the other side. Repeat 5 times.

