PORTAL VEIN THROMBOSIS IN CHILDREN & YOUNG ADULTS
Patient Education Material
The portal vein is a blood vessel that carries blood from the gastrointestinal tract, gallbladder, pancreas, and spleen to the liver. This blood contains nutrients and toxins extracted from digested contents. Approximately 75% of total liver blood flow is through the portal vein, with the remainder coming from the hepatic artery. The blood leaves the liver to the heart in the hepatic veins.

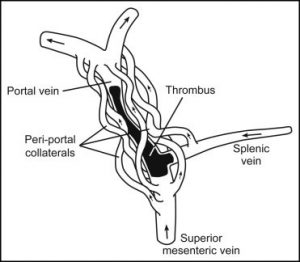
Portal vein thrombosis
Portal vein thrombosis (PVT) the blockage of the portal vein with blood clots. In fact, some believe that there 1% lifetime risk of PVT in the general population. The diagnosis can now be readily established by using an ultrasound scan or CT or scans.
There various causes of PVT, but whatever the cause, the sequence of events very seriously. Patients may present with severe bleeding from esophageal or gastric varices. The two main types of PVT are acute and chronic.

PVT not very uncommon in Pakistan. One of the common causes of belly button infection in infancy. The infection leads to clotting in the portal vein. Most of the time this goes unnoticed and the diagnosis is only made when a child presents with gastrointestinal bleeding. Other causes of portal vein thrombosis are;
Causes of congenital portal vein thrombosis
Deficiency or access of certain chemicals in the body can increase the risk of blood clotting in the veins. Some of these abnormalities are present from birth.
| Inherited prothrombotic disorders
· ☐ Factor V Leiden mutation · ☐ Factor II gene mutation · ☐ Protein C deficiency · ☐ Protein S deficiency · ☐ Antithrombin III deficiency |
| Acquired thrombophilic disorders
· ☐ Primary myeloproliferative disorders · ☐ Paroxysmal nocturnal hemoglobinemia · ☐ Antiphospholipid syndrome · ☐ Hyperhomocysteinemia · ☐ Increased factor VIII levels · ☐ Thrombin activatable fibrinolysis inhibitor gene |
Symptoms of portal vein thrombosis
Portal hypertension and its consequence of bleeding vary usually seen in people with portal vein thrombosis.
As the blood tries to find another way back to the heart, new blood vessels open up. Among these vessels are those that run along the wall under the lining of the upper part of the stomach and the lower end of the esophagus (food pipe). These veins protrude into the gullet and the stomach and can bleed. The dilated veins in the gullet known as varices. Bleeding may be a gentle ooze in which case anemia the commonest symptom. Sometimes there can be a major bleed; a child may have a hemorrhage and either vomit blood or passes blood through their bowels. This blood may appear to be black since it often changed as it passes through the body.
Oesophageal varices represent a significant complication of portal vein thrombosis.
Detection of varices
Unless they bleed, varices do not produce any complications or symptoms. The only way they can be detected is by a process called endoscopy. During endoscopy, a small flexible tube put into the gullet and the endoscopist can see not only where the varices present but also their size.
Prevention of bleeding
In general, small varices rarely bleed and bigger ones may bleed. Small varices however, may well develop into large varices over time. For those children who have varices and likely to bleed, treatment with drugs can sometimes reduce the risk of bleeding and reduce the severity of any bleed should it occur. The drug most commonly used propranolol. As with all drugs, not everyone suitable and some have side-effects. Alternative methods may sometimes be used for those who at risk of bleeding.
Treatment
Current treatments do allow for early identification of those people who at risk of variceal bleeding, and treatments can greatly reduce the risk and severity of the bleeds. For those who have bleeding oesophageal varices, this a medical emergency but early treatment usually highly effective. There a variety of approaches to treat bleeding varices and the treatment used will depend on the overall condition of the patient.
Propranolol used both for the prevention of bleeding and also in those people who have bled. It may be used in the prevention of re-bleeding. A number of treatment options available for the treatment and prevention of bleeding.
Drugs
Several drugs useful in the treatment of variceal bleed. These drugs, such as glypressin or octreotide, given by injection.
Endoscopic techniques
- Banding– with banding techniques a single vein (the varix) is sucked into a ring at the end of the endoscope. A small band is placed around the base of the varix. After one or two days this will result in the formation of a clot which will control the bleeding.
- Injection scleropathy – this a sclerosant (special chemical) material injected into the veins of the gullet. It done after you given some sedation and a camera (endoscope) has been passed into your gullet. A fine flexible needle passed through the endoscope and used to inject the sclerosant material into the oesophageal veins or the adjacent veins. These injections cause clotting and will also stimulate some scarring to reduce the recurrence of varices.
Treatment of portal vein thrombosis (PVT)
There various forms of treatment modalities for PVT, these include medical and surgical.
Medical treatment
The mainstay of treatment to minimize portal hypertension and to avoid progression of thrombosis (clot in the portal vein) by;
1-Anticoagulation (blood thinning medications). Spontaneous recovery with re-canalization of the portal vein can be achieved in near half of the patients with anticoagulation.
2-Endoscopic intervention (banding or sclerotherapy) for bleeding varices.
3-Drug therapy (propranolol) to reduce portal hypertension.
Surgical shunts
The patients that do not respond to the medical therapy may require surgical intervention if they suffer from persistent complications of portal hypertension. Variceal bleed a common and disastrous complication.
Surgical options for PVT are portosystemic shunts. The choice of procedure depends on the patient’s overall condition and liver status. Liver transplant only considered for patients who severe scarring (cirrhosis) of the liver. That patient whose liver function is normal; they good candidate for surgical shunts.
The shunting procedures available;
- Splenorenal shunt
- Mesocaval shunt
- Portocaval shunt
It believed that the shunt operation very effective in controlling the risk of bleeding in long term.

Outlook
Portal vein thrombosis not a rare disease but it carries serious complications if left untreated. The surgical options for PVT are simple and carry a good prognosis when performed at right time. All the procedures carry certain risks but the procedure of choice dependent on the patient‘s condition. Variceal bleeding a serious complication that requires urgent management and monitoring. These patients should be looked after only by experienced doctors at specialist centers.
If you have any further questions or worries please feel free to ask the staff on your ward, your surgical team or your clinical nurse specialist.
Patient Help Line (PHL)
Patient Help Line (PHL) a service that offers support, information and assistance to patients, relatives and visitors. They can also provide help and advice if you have a concerns.
Transplant coordinator:
Mr. Touseef Ahmed 0333-1027353
Transplant Coordinator: (for post-transplant follow up patients):
M. Zaheen Hashmi 0333-1027354
Hepatobiliary & Pancreatic Surgery Services:
Muhammad Asif 0341-0543883
24 Hours Patients emergency Helpline: 0333-1027356
Email: info@faisaldar.com
Counselling service: The counselling service offers free and confidential sessions to our inpatients, outpatients, their relatives and friends. If you would like to meet with one our counsellors you can contact us on 0333-1027356
Transplant coordinator:
Mr. Touseef Ahmed 0333-1027353
Transplant Coordinator: (for post-transplant follow up patients):
M. Zaheen Hashmi 0333-1027354
Hepatobiliary & Pancreatic Surgery Services:
Muhammad Asif 0341-0543883
24 Hours Patients emergency Helpline: 0333-1027356
Email: info@faisaldar.com
Website: www.faisaldar.com
Duct injuries during Gallbladder surgery:
In about 10% to 30% of cases, bile duct injuries are found by the doctor at the time of surgery. He or she might notice leaking bile or blockage by sight or by using a test called intraoperative cholangiography (IOC). IOC is an X-ray exam of the bile ducts after a dye is injected to make the flow of bile clearly visible on the X-ray image.
If your injury was not found during surgery, tests your doctor might use to help diagnose a bile duct injury include:
- Abdominal ultrasound: This test uses sound waves and echoes to create images of the organs in the abdomen.
- Endoscopic retrograde cholangiopancreatography (ERCP): This test uses alighted. Flexible scope inserted into the upper part of the digestive system to look at and take X-rays of the bile ducts. Sometimes, bile duct injuries can also be treated using ERCP.
- Percutaneous transhepatic cholangiography (PTC): Like IOC, during this test, X-rays are taken after a dye is injected into the bile ducts.
- Magnetic resonance cholangiopancreatography (MRCP): This test uses magnetic resonance imaging, which uses a large magnet and radio waves to create images of the inside of the body, to view the bile ducts.
Bile Duct injuries from Gallbladder surgery treated:
If you’re experiencing any of the symptoms of bile duct injury after gallbladder surgery. it’s important to seek proper evaluation and treatment from a healthcare expert experienced in the diagnosis and treatment of bile duct injuries, as well as other hepatobiliary conditions.
The first goal of treatment is to manage any infection, leakage, or blockage caused by the injury. Then, the doctor may need to reconstruct the bile duct, often using a piece of intestine to bypass the blockage or the area where the duct was cut or burned.

The outcome depends on the type and extent of the injury and how soon the injury is found. Most bile duct injuries can successfully be repaired, and the patient can go on to a good quality of life. In severe cases, with more than one surgery, many months of recovery might need.
Kindly contact:
-
One PKLI Avenue, DHA, Phase-6, Lahore, Pakistan.
-
+92 42 111 117 554

