THROMBECTOMY
Patient Education Material
An endovascular thrombectomy is the removal of a thrombus (blood clot) under image guidance. A thrombectomy is most commonly performed for an arterial embolism, which is an arterial blockage often caused by atrial fibrillation, a heart rhythm disorder. An arterial embolism causes acute limb ischaemia (restricted blood supply) which leads to pain in the affected area. A thrombectomy can also be used to treat conditions in your organs, such as in your liver or kidney.
Your doctor may recommend that you have a thrombectomy as a treatment for stroke or for mesenteric ischaemia, where the blood flow in your small intestine is restricted due to inflammation or injury.
The interventional radiologist will insert a 3 mm plastic tube (called a sheath) into the base of your skull or your groin. They will guide the sheath to the blood clot.
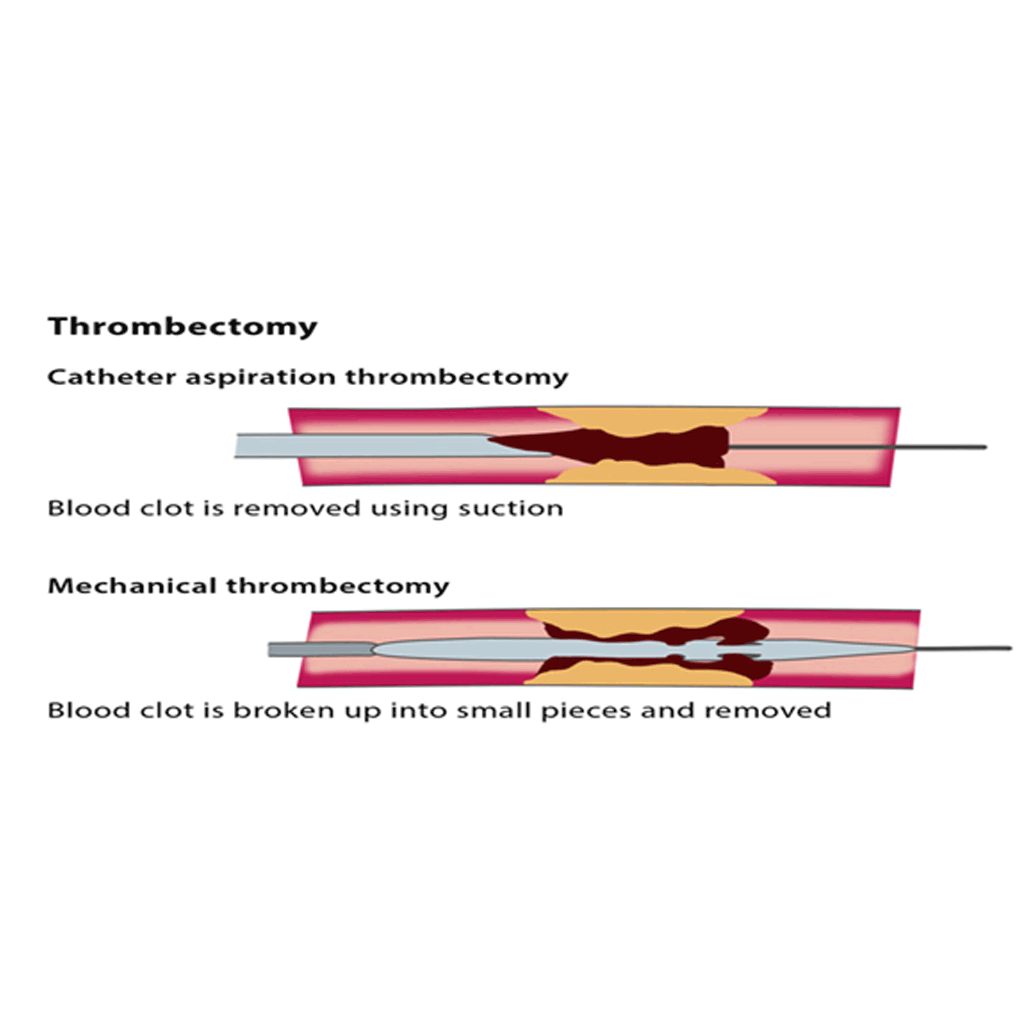
There are a number of different techniques for this procedure. The blood clot can be removed using a vacuum to suck the thrombus out, or mechanical equipment to break up the clot, or with clot using saline jets or ultrasound waves.
The devices for these techniques are inserted over the sheath into the affected artery. You may also need additional catheter thrombolysis, a procedure in which clot-dissolving medication is delivered to the clot under X-ray imaging.
A combined treatment using both thrombectomy and thrombolysis can continue over 24-48 hours with several follow-ups using angiography at regular intervals.
An interventional thrombectomy is used to remove the blood clot and to avoid a permanent blockage in the vein or artery which would prevent blood flow to a limb or an organ, causing acute symptoms of pain, lack of a pulse, paleness, paraesthesia (when a limb ‘falls asleep’) and paralysis, as well as the possibility of permanent complications such as the death of tissue cells in your body.
A thrombectomy is often combined with other treatments, such as treatment to stop blood clots forming or thrombolysis, which involves using medication to break the blood clot down and is followed by strict observation for 24-48 hours.
You will also be treated for the underlying condition which caused the arterial thrombus, such as a heart rhythm disorder or a small blood clot caused by deep venous thrombosis.
Minor risks include the risk of bruising at the puncture site in the neck or groin or in the affected limb. Major risks include the risk of the blood clot travelling deeper into the artery or vein or an injury to the affected area during the treatment.
In rare cases, patients experience bleeding in the skull as a result of the combined thrombectomy and thrombolysis – if this occurs, the treatment must be stopped immediately.
- Ansel GM, George BS, Botti CF, McNamara TO, Jenkins JS, Ramee SR, et al. Rheolytic thrombectomy in the management of limb ischemia: 30-day results from a multicenter registry. Journal of endovascular therapy: an official journal of the International Society of Endovascular Specialists. 2002; 9(4):395-402.
- Allie DE, Hebert CJ, Lirtzman MD, Wyatt CH, Keller VA, Khan MH, et al. Novel simultaneous combination chemical thrombolysis/rheolytic thrombectomy therapy for acute critical limb ischemia: the power-pulse spray technique. Catheterization and cardiovascular interventions: official journal of the Society for Cardiac Angiography & Interventions. 2004; 63(4):512-22.
- Kasirajan K, Gray B, Beavers FP, Clair DG, Greenberg R, Mascha E, et al. Rheolytic thrombectomy in the management of acute and subacute limb-threatening ischemia. Journal of vascular and interventional radiology: JVIR. 2001; 12(4):413-21.
- Kasirajan K, Haskal ZJ, Ouriel K. The use of mechanical thrombectomy devices in the management of acute peripheral arterial occlusive disease. Journal of vascular and interventional radiology: JVIR. 2001; 12(4):405-11.
- Wagner HJ, Muller-Hulsbeck S, Pitton MB, Weiss W, Wess M. Rapid thrombectomy with a hydrodynamic catheter: results from a prospective, multicenter trial. Radiology. 1997; 2 05(3):675-81.
Kindly contact:
- One PKLI Avenue, DHA, Phase-6, Lahore, Pakistan.
- info@pkli.org.pk
- +92 42 111 117 554

